Abstract
Background. The Lesbian, Gay, Bisexual, Transgender, and Queer individuals frequently encounter disparities in healthcare access, quality and inclusivity. Despite growing awareness of these challenges, Poland has lacked a psychometrically validated tool to assess the experiences of sexual and gender minorities in clinical settings.
Objectives. This study aimed to develop and validate the LGBTQ+ Healthcare Experiences Scale (LGBTQ+ HCES) tailored to the Polish context.
Materials and methods. A multi-phase cross-sectional study was conducted in 2025. The initial pool of items was developed through a narrative literature review and refined by 4 researchers with clinical and academic experience in LGBTQ+ health. Content validity was assessed using a 2-round Delphi process involving a multidisciplinary panel of experts (n = 12), who rated item clarity and relevance using Aiken’s V. A pilot test with 30 LGBTQ+ participants confirmed comprehension and technical usability. The final 15-item instrument, comprising 3 subscales (Respect and Inclusivity, Discrimination and Microaggressions, Trust and Comfort), was administered to 172 LGBTQ+ individuals recruited via social media. Psychometric evaluation included descriptive analysis, confirmatory factor analysis (CFA) and reliability testing (Cronbach’s α, McDonald’s ω).
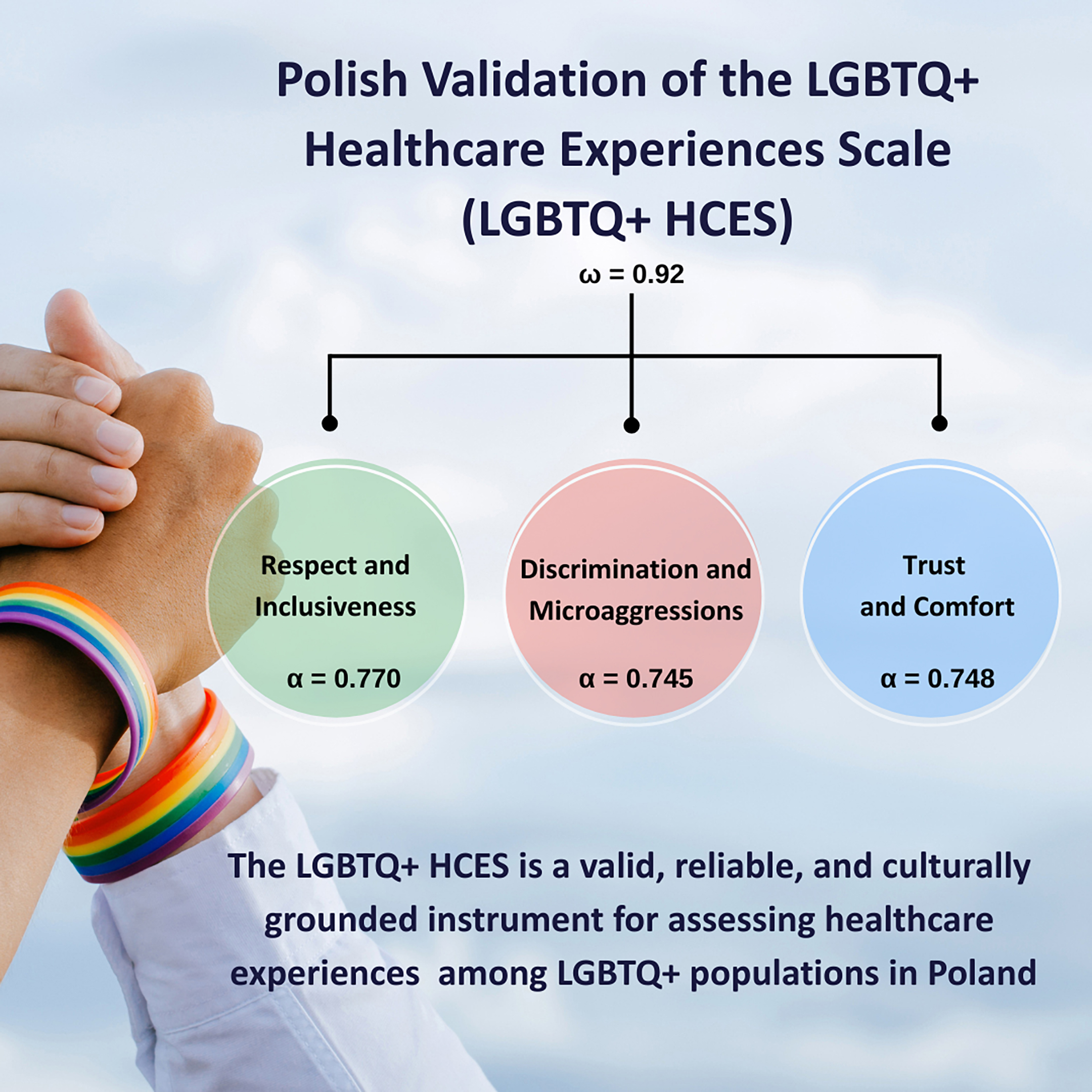
Results. Confirmatory factor analysis supported a 3-factor model comprising Respect and Inclusivity, Discrimination and Microaggressions, and Trust and Comfort. Model fit indices met recommended thresholds (root mean square error of approximation = 0.041, standardized root mean square residual = 0.057, comparative fit index = 0.998). All subscales demonstrated acceptable to strong internal consistency (α = 0.745–0.778; ω = 0.92). No significant floor or ceiling effects were found to compromise the scale’s performance. All items showed positive item-total correlations and contributed meaningfully to their respective subscales.
Conclusions. The LGBTQ+ HCES is a valid, reliable and culturally grounded instrument for assessing healthcare experiences among LGBTQ+ populations in Poland. It holds promise for research, public health surveillance and health system quality improvement efforts to promote inclusive and equitable care.
Key words: health equity, LGBTQ+ health, healthcare experiences, inclusivity in healthcare
Background
Sexual and gender minorities (SGM) – including lesbian, gay, bisexual, transgender, queer, and other non-heteronormative identities (LGBTQ+) – face disproportionate barriers to accessing equitable, culturally competent and respectful healthcare globally.1 These disparities are not isolated incidents, but rather the result of entrenched systemic discrimination, institutional neglect and a lack of clinician preparedness to deliver inclusive care.1, 2 Across health systems, LGBTQ+ individuals are more likely to report experiences of microaggressions, heteronormative assumptions, diagnostic overshadowing, and outright mistreatment.3, 4 These interactions contribute to widespread healthcare avoidance, psychological distress, and worse outcomes in both mental and physical health domains.5, 6
In Central and Eastern Europe, and Poland in particular, these disparities are amplified by hostile sociopolitical climates that institutionalize stigma and marginalization.7 International Lesbian, Gay, Bisexual, Trans and Intersex Association (ILGA)-Europe’s 2025 Rainbow Europe Index ranked Poland last among 49 countries regarding LGBTQ+ equality, highlighting a stark regression in legal protection, public policy and social acceptance.8 Over the past decade, Polish authorities have promoted exclusionary rhetoric, established so-called “LGBT-free zones,” and restricted public expressions of LGBTQ+ identity, including pride marches and education campaigns.7, 9 These structural conditions cultivate fear, social invisibility and medical mistrust, particularly in healthcare settings that are often perceived as unsafe or overtly discriminatory.10
Evidence from high-income countries suggests that LGBTQ+ patients often internalize prior negative experiences with clinicians, leading to chronic underutilization of services, delays in diagnosis and a reluctance to disclose identity in clinical contexts.11, 12, 13 In Poland, however, these patterns remain under-researched. Despite increasing international recognition of LGBTQ+ health disparities, few tools exist to systematically assess the lived healthcare experiences of LGBTQ+ individuals in culturally specific, non-English-speaking settings. This gap limits the development of local data-driven interventions and the ability to monitor progress toward equity-based health system reform.
While several instruments assessing healthcare professionals’ competence in working with LGBTQ+ populations have been developed and validated in Poland, there remains a critical gap in tools that capture the patient perspective.14 Specifically, no validated instrument currently exists to assess how LGBTQ+ individuals themselves perceive respect, discrimination and emotional safety during clinical encounters. Internationally, only a few patient-centered instruments have been developed to assess LGBTQ+ individuals’ experiences in healthcare. For example, the Sexual Stigma in Health-Care Services Scale, recently validated in Taiwan, focuses on the experiences of gay and bisexual men.15 However, this tool remains population-specific and does not provide a comprehensive measure of healthcare experiences across the broader LGBTQ+ community. This patient-centered perspective is essential for understanding the full scope of healthcare (in)equity and informing interventions aimed at system-level change in the Polish context.
Objectives
This study aimed to develop and validate the Lesbian, Gay, Bisexual, Transgender, and Queer+ Healthcare Experiences Scale (LGBTQ+ HCES), a self-report instrument designed to assess the quality, inclusivity, and safety of healthcare experiences among LGBTQ+ individuals in Poland.
Materials and methods
Design
This study employed an instrumental design, as described by Montero and León,16 which focuses on developing measurement tools – including item construction and psychometric validation. The research aimed to create and validate a novel self-report instrument to assess the healthcare experiences of LGBTQ+ individuals in Poland.
Item development
The initial development of the LGBTQ+ HCES took place between January and February 2024. A narrative literature review was conducted to identify existing instruments and conceptual frameworks related to LGBTQ+ patient experiences. Although several tools exist to assess healthcare providers’ cultural competence, no validated, patient-centered instruments were available in the Polish context at the time of the study. The preliminary pool of items was generated through collaborative discussions among 4 researchers with expertise in LGBTQ+ health, health psychology and public health. These items were grounded in existing theoretical models, including the minority stress framework, structural stigma theory and prior empirical studies focusing on LGBTQ+ individuals’ interactions with healthcare systems. Each author contributed to conceptualizing the scale domains, item drafting and the review process. A total of 15 items were developed to capture key dimensions such as respect and inclusivity, experiences of discrimination and microaggressions, and emotional safety and trust in clinical encounters. Items were designed to be brief, culturally relevant and linguistically appropriate for Polish-speaking respondents.
Selection of experts
A panel of 12 multidisciplinary experts was recruited to evaluate the content validity of the LGBTQ+ HCES. Experts were defined as professionals with a minimum of 5 years of clinical or academic experience in health-related fields and documented engagement in LGBTQ+ health, human rights or public health practice. The panel included: a psychiatrist, psychologist, family physician, psychotherapist, paramedic, dietitian, nurse, public health specialist, pharmacist, physiotherapist, laboratory diagnostician, and a patient representative from the LGBTQ+ community.
Experts were invited via email, and the invitation included a cover letter outlining the study’s goals, the rationale for developing the scale, the selection criteria for participation, and ethical assurances concerning confidentiality, data protection and voluntary participation. Each expert received an information sheet describing the questionnaire structure and participation instructions.
The expert evaluation process was conducted through an online form hosted on Webankieta.pl, a secure Polish data collection platform. Before beginning their review, all participants provided informed consent electronically, which was in line with national data protection regulations. Participation was anonymous, confidential and voluntary.
Delphi method
A conventional Delphi method was employed to evaluate the content validity of the LGBTQ+ HCES, involving 2 structured rounds of expert consultation.17 This approach, widely used in instrument development, facilitates consensus-building among experts while allowing for iterative refinement of questionnaire items. Following the recommendations of Linstone and Turoff,18 2 rounds were deemed sufficient to ensure informed agreement among participants. The Delphi process was conducted in March 2024, during the 1st month of the study. In Round 1, experts were asked to assess each item for content relevance and linguistic clarity using a 5-point Likert scale (1 = not at all; 5 = completely). Additionally, qualitative feedback was collected through open-ended comment boxes, where panelists could suggest modifying item structure, language or conceptual scope. This feedback was reviewed in detail, and items requiring revision were adjusted accordingly. In Round 2, experts re-evaluated the modified items using the same procedure. This round confirmed whether the revisions enhanced clarity and relevance, and whether consensus had improved. All items in the final version met the predefined inclusion thresholds (Aiken’s V ≥ 0.75), and no further changes were deemed necessary. Initially, invitations were sent to 16 experts, covering all predefined disciplines. Four invitees either did not return the survey or provided incomplete responses, and were therefore excluded from the Delphi process. The final expert panel consisted of 12 members. All 12 completed both Delphi rounds, yielding a 100% response rate in the qualified panel. Communication with the panel was conducted via email, and both Delphi rounds were administered using a secure online survey platform (https://www.webankieta.pl/). No experts were lost between rounds; full participation was retained throughout the process.
Content validity analysis
The content validity of the questionnaire was assessed using Aiken’s V coefficient, a widely used index for evaluating the relevance and clarity of individual items based on expert ratings. Each expert rated every item using a 5-point Likert scale (1 = not at all relevant/clear; 5 = completely relevant/clear). Aiken’s V was calculated for each item using the standard formula:
V = (X − l)/k,
where X is the mean of expert ratings, l is the lowest possible rating (1), and k is the range of the scale (4, for a 1–5 scale). A threshold of Aiken’s V ≥ 0.75 was used to indicate acceptable content validity. Items scoring below this value in the first round were revised before re-evaluation. All calculations were conducted in Microsoft Excel 2013 (Microsoft Corp., Redmond, USA).
Comprehensibility analysis and linguistic validation
In both rounds of expert review, participants were asked to assess the content relevance and the linguistic clarity of each item. Ratings were provided on a 5-point Likert scale (1 = unclear, 5 = completely clear). Items receiving lower clarity scores in the 1st round – particularly those with Aiken’s V < 0.75 – were revised for improved wording. In the 2nd round, experts re-evaluated the revised items.19, 20 This 2-step process allowed for refinement of item phrasing based on expert feedback to ensure that all items were linguistically clear and culturally appropriate for the Polish context. No items required further revision after the 2nd round, as all reached acceptable clarity levels.
Instrument description
The LGBTQ+ HCES is a 15-item self-report questionnaire developed to assess the healthcare experiences of LGBTQ+ individuals within the Polish healthcare system. The tool was designed to evaluate how affirming, respectful and safe these interactions were, particularly in terms of inclusivity, perceived discrimination and emotional comfort when disclosing one’s sexual orientation and/or gender identity.
The items reflect 3 key dimensions: 1) Respect and Inclusivity, which addresses whether patients felt acknowledged and valued regardless of their identity; 2) Discrimination and Microaggressions, which captures instances of subtle or overt exclusion, bias or inappropriate language from healthcare providers; and 3) Trust and Comfort, which assesses the extent to which respondents felt emotionally safe and supported in clinical encounters. Responses are rated on a 7-point Likert scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”), with 5 negatively worded items reverse-coded to ensure higher scores consistently represent more positive healthcare experiences. Subscale scores are computed by averaging the relevant items, and an overall mean score is derived to reflect general experiences across domains.
The instrument used gender-inclusive and non-binary-affirming language to promote psychological safety and accommodate diverse gender identities. Respondents are invited to reflect on direct and perceived experiences, regardless of whether their LGBTQ+ identity was disclosed to medical personnel.
For transparency, all 15 questionnaire items are shown in their English translation in the Results section. The original Polish version of the LGBTQ+ HCES is provided in the raw data to support further validation and implementation efforts. The finalized version of the LGBTQ+ HCES was pilot-tested among 30 participants using an online survey (https://www.webankieta.pl/). The aim was to evaluate the clarity of item wording and the technical functionality of the questionnaire. No comprehension issues or technical difficulties were reported. The platform’s built-in IP filtering system was used to identify potential duplicate entries; none were detected. To further minimize the risk of duplicate or invalid responses, the platform also applied completeness checks and time monitoring. Additionally, all responses were screened for internal consistency, and no irregular patterns were detected.
Main study design and participants
A cross-sectional study was conducted between April and May 2024 using convenience sampling via social media platforms, including Instagram and a closed Facebook group for the LGBTQ+ community. Participants were eligible if they were aged 18 years or older, self-identified as LGBTQ+ and had accessed healthcare services in Poland within the past 24 months (including primary care, emergency departments, hospitalizations, diagnostic testing, ambulance services, or private healthcare).
All participants provided informed consent before participation. The survey was fully anonymous and voluntary, and participants were informed that they could withdraw anytime without giving a reason.
A total of 172 participants were enrolled. Sample size determination followed recommendations suggesting 5–10 participants per item for psychometric validation. Given the 18-item structure, a minimum of 90–180 respondents was targeted, which aligns with Argimon-Pallàs’s guidelines.21 The study was conducted by the Declaration of Helsinki and approved by the Bioethics Committee of Wroclaw Medical University, Poland (approval No. KB 976/2022). This research is part of the Health Exclusion Research in Europe2 (HERE2) project.
Statistical analyses
Internal consistency of the questionnaire was checked with confirmatory factor analysis (CFA). Standardized root mean square residual (SRMR), root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker–Lewis index (TLI) were used within the Hu–Bentler 2-index strategy to assess the goodness of fit of the CFA model (criteria: SRMR < 0.09 plus at least 1 of the following: CFI > 0.96, TLI > 0.96, or RMSEA < 0.06). Cronbach’s α and discriminative power index were internal consistency measures. The following thresholds for internal consistency were used: 0.9 ≤ α – excellent; 0.8 ≤ α < 0.9 – good; 0.7 ≤ α < 0.8 – acceptable; 0.6 ≤ α < 0.7 – questionable; 0.5 ≤ α < 0.6 – poor; and α < 0.5 – unacceptable. R 4.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and RStudio (https://posit.co/products/open-source/rstudio/?sid=1) GUI and psy,22 lavaan,23 psych,24 and diagram packages25 were used.
Results
Sociodemographic characteristics
A total of 172 individuals participated in the study. The mean age was 30.95 years (standard deviation (SD) = 8.69). Nearly half of the sample identified as cisgender men (47.67%) and almost 1/3 as cisgender women (29.65%), with a notable proportion identifying as non-binary (11.63%). The majority reported a homosexual orientation (69.77%). Most participants lived in large urban areas (>500,000 inhabitants) and held at least a secondary education, with over 30% having a master’s degree. Detailed sociodemographic characteristics are presented in Table 1.
Instrument outcomes
Mean scores across the LGBTQ+ HCES and its 3 subscales suggest moderately positive healthcare experiences within the sample, though with considerable variability (Table 2). The highest mean was observed for Respect and Inclusiveness (mean (M) = 25.56, SD = 5.93), while Discrimination and Microaggressions showed the lowest (M = 16.41, SD = 7.24), indicating unequal exposure to negative experiences.
Analysis of the individual questionnaire item
Descriptive item-level analysis revealed high ceiling effects for items 2 and 5, with 57.6% and 50.0% of respondents selecting the maximum response (Table 3). This suggests these items may have limited discriminative capacity in this sample. While this could indicate redundancy, it is also possible that these items tap into universally positive experiences that are crucial to the construct and were designed to function as intentional “anchor” or “booster” items. In contrast, item 15 showed the highest floor effect (31.4%), potentially pointing to problematic or poorly experienced care domains.
Confirmatory factor analysis
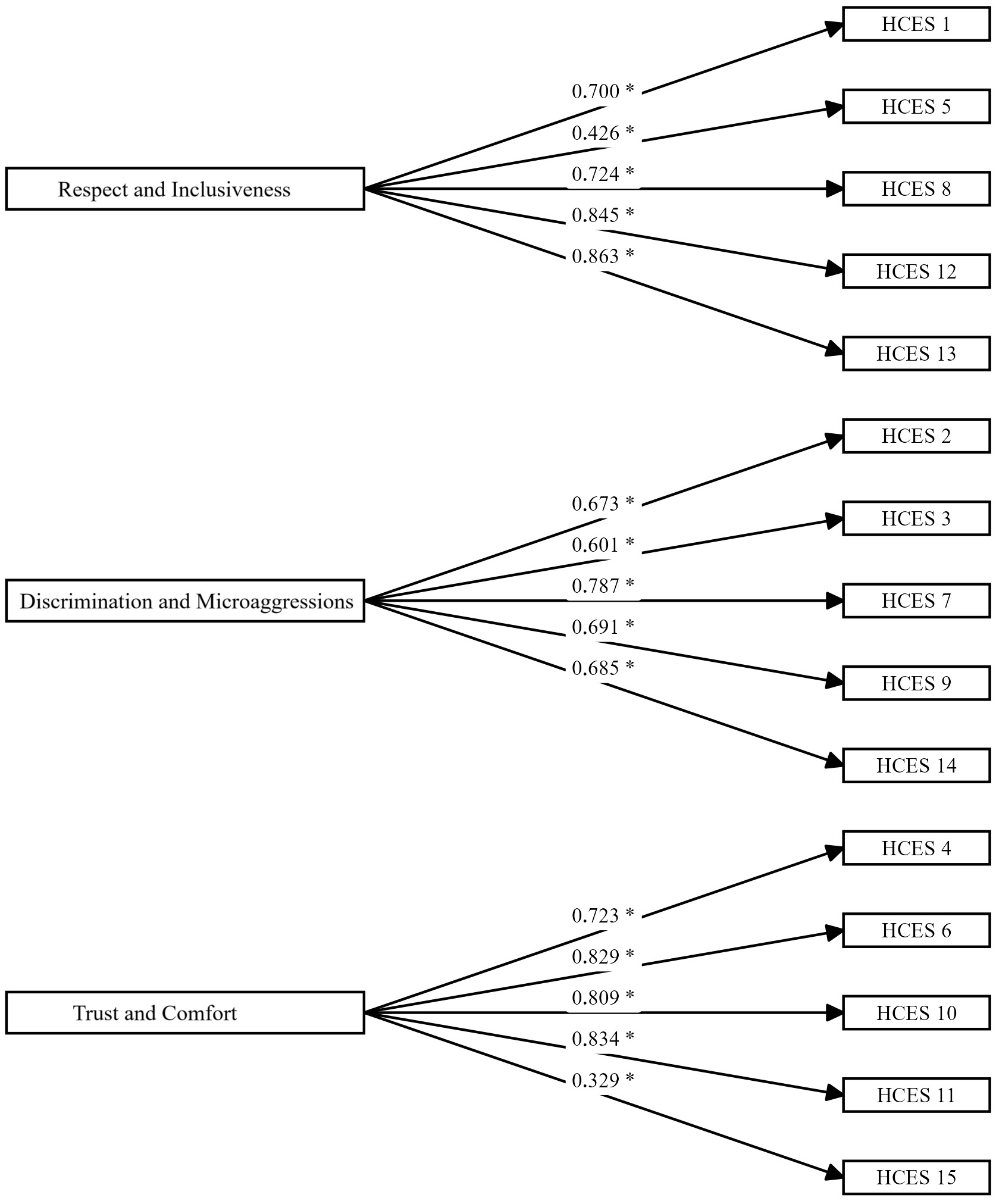
The HCES items are measured on an ordinal scale, and the Diagonally Weighted Least Squares (DWLS) estimator was used for CFA. The initial 3-factor model (Model I) showed suboptimal fit indices. Correlations between selected item pairs within the same factor were added to improve model fit based on modification indices. The revised model (Model II) showed improved fit and met recommended thresholds (SRMR < 0.08, RMSEA < 0.06, CFI > 0.95). These adjustments preserved the original factor structure of the HCES. Detailed results are presented in Table 4.
Internal consistency analysis of the LGBTQ+ HCES
All item loadings were statistically significant (p < 0.001), ranging from 0.329 to 0.863, indicating adequate association with their respective subscales. Cronbach’s α coefficients showed acceptable internal consistency across the 3 subscales: Respect and Inclusiveness (α = 0.770), Discrimination and Microaggressions (α = 0.745) and Trust and Comfort (α = 0.778). McDonald’s ω index (ω = 0.92) further confirmed the strong internal consistency of the scale.
Item-level reliability analysis revealed no substantial gains in α values upon removal of any item. Although minor increases were observed for Item 5 and Item 15 within their respective subscales, these changes were insufficient to justify item deletion. All items demonstrated positive item-total correlations, supporting their contribution to internal consistency. Detailed results for item loadings and internal consistency are presented in Table 5, with additional reliability metrics shown in Table 6. The path diagram for the CFA of the LGBTQ+ HCES is illustrated in Figure 1.
Discussion
To our knowledge, this study presents the first validated, patient-centered instrument in Poland explicitly designed to capture the healthcare experiences of LGBTQ+ individuals. The LGBTQ+ HCES demonstrated strong psychometric properties, including acceptable internal consistency across all subscales and excellent model fit indices, supporting its use as a reliable tool in research and applied settings.
The final version of the scale, encompassing 3 dimensions – Respect and Inclusivity, Discrimination and Microaggressions, and Trust and Comfort – closely reflects conceptual frameworks rooted in the minority stress model and structural stigma theory. These dimensions have also been identified in previous studies as key determinants of healthcare quality and access for SGM populations.2, 26, 27, 28 Importantly, our findings indicate that even within a relatively young, urban and highly educated LGBTQ+ cohort, negative clinical experiences remain common, with notably lower scores in perceived discrimination and provider competence.
The high internal consistency and robust factor structure suggest that the LGBTQ+ HCES successfully captures distinct but interrelated aspects of the patient experience. The Discrimination and Microaggressions subscale, which yielded the lowest mean score, underscores the persistence of subtle and overt biases in Polish healthcare settings. This finding aligns with international literature demonstrating the pervasiveness of microaggressions – often invisible to cisgender and heterosexual providers – such as inappropriate assumptions, invalidation of identity or reluctance to use inclusive language.29, 30
Conversely, the Respect and Inclusivity subscale had the highest score, suggesting that some interpersonal aspects of care – particularly overt disrespect or denial of identity – may be less prevalent. However, the relatively high ceiling effects on items related to being treated respectfully may also reflect limited item sensitivity or social desirability bias.
The Trust and Comfort subscale revealed moderate scores, consistent with studies showing that even when overt discrimination is absent, LGBTQ+ patients frequently report discomfort disclosing their identities or anticipating poor treatment.2, 12, 15, 26 This has critical implications for clinical care: nondisclosure is associated with reduced diagnostic accuracy, inappropriate treatment plans and poor health outcomes, particularly in mental health, sexual health and chronic disease management.31, 32, 33 Item 15 within this subscale demonstrated the highest floor effect (31.4%). This finding likely reflects structural barriers in the Polish healthcare system, where information about LGBTQ+-affirmative providers remains scarce and often inaccessible. Although the item showed lower factor loading and item–total correlation compared to other items, it was retained due to its conceptual relevance: knowing where to find inclusive services is a critical dimension of comfort and trust in healthcare. Importantly, the overall reliability of the subscale remained acceptable, indicating that inclusion of this item did not compromise the psychometric integrity of the instrument.
While several instruments assess healthcare provider competencies toward LGBTQ+ patients (e.g., the LGBT-DOCSS, the GAP), these tools do not capture the patients’ perspectives.2, 34 The LGBTQ+ HCES fills this gap in Poland, where widespread institutional hostility and sociopolitical marginalization exacerbate mistrust toward healthcare services.7, 8, 35
Practical implications
The validated LGBTQ+ HCES provides a robust, culturally relevant instrument for assessing the healthcare experiences of sexual and gender minorities in Poland. Its practical applications span clinical, administrative and policy levels. The scale enables routine monitoring of inclusivity and patient-centeredness in clinical settings, offering insight into perceived respect, safety and discrimination. Facilities may use subscale scores to identify specific domains – such as fear of disclosure or lack of cultural competence – that require targeted interventions. At the healthcare system level, the tool can facilitate equity-focused audits and inform continuous quality improvement initiatives. Integration into national health reporting frameworks would allow for standardized benchmarking and longitudinal tracking of LGBTQ+ patient experiences across regions and care settings. The LGBTQ+ HCES may also serve as an outcome measure in intervention studies, evaluating the impact of inclusivity training or structural reforms (e.g., removal of binary intake forms). Finally, it offers a means of amplifying community voice, enabling LGBTQ+ individuals to report health system performance based on lived experience. By translating subjective experiences into measurable data, the LGBTQ+ HCES provides the empirical foundation needed to guide responsive, equity-driven health system reforms in settings where LGBTQ+ health remains politically contested and structurally neglected. Beyond Poland, the LGBTQ+ HCES also holds potential for cross-cultural adaptation. Applying the scale in other healthcare systems would allow for standardized international comparisons of LGBTQ+ patients’ experiences, facilitating both the identification of universal barriers and the recognition of context-specific challenges. Such comparative research could strengthen the global evidence base needed to inform inclusive and equity-driven healthcare reforms. This makes the LGBTQ+ HCES particularly valuable for use in countries with sociopolitical contexts comparable to Poland, where LGBTQ+ health remains under-researched and marginalized.
Limitations
This study has several limitations. First, participants were recruited through convenience sampling on social media platforms, which may limit representativeness to LGBTQ+ individuals who are active online and engaged in digital communities. As a result, the findings may not fully reflect the experiences of those with limited internet access or those less connected to LGBTQ+ networks. Second, self-report questionnaires introduce the potential for social desirability or recall bias. Lastly, while the scale demonstrated strong psychometric properties in the Polish context, future studies may explore its test–retest reliability and sensitivity to change over time in intervention-based research.
Conclusions
The LGBTQ+ HCES demonstrated strong psychometric properties, including robust content validity, high internal consistency, and good model fit. The tool captures 3 core dimensions of LGBTQ+ individuals’ experiences in the healthcare system: Respect and Inclusivity, Discrimination and Microaggressions, and Trust and Comfort in clinical settings.
The LGBTQ+ HCES provides a reliable and practical measure for evaluating healthcare experiences among sexual and gender minorities in Poland. It is suitable for academic research and public health applications, health system evaluation and equity-focused service improvement. The scale is intended to inform efforts to identify and address healthcare inequities affecting LGBTQ+ populations and support interventions to enhance inclusivity and responsiveness in clinical practice. Its adoption in health systems and research settings may contribute to more inclusive policy development and patient-centered care for LGBTQ+ populations.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in Zenodo at https://doi.org/10.5281/zenodo.17026585.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
OpenAI’s ChatGPT was used for language editing and proofreading to ensure the final manuscript’s clarity, coherence, and linguistic accuracy.