Abstract
The SAPIENCE study explores the long-term psychological, social, and systemic challenges faced by caregivers of individuals with NMDAR encephalitis. It aims to inform patient- and caregiver-centered strategies that support recovery and wellbeing.
Key words: rare diseases, patient-centered care, multidisciplinary team, social & caregiver burden, autoimmune encephalities
Introduction
N-methyl-D-aspartate receptor (NMDAR) encephalitis is a rare autoimmune disorder that affects the central nervous system, often leading to severe neuropsychiatric symptoms. It has an estimated annual incidence of 1.5 cases per million people and a prevalence of 0.6 per 100,000 individuals, primarily affecting young adults, with a median onset age of 21 years.1 This disorder is characterized by a complex clinical presentation that can include psychiatric disturbances, cognitive impairment, movement disorders, autonomic instability, and seizures. Due to its heterogeneous and often initially misleading symptoms, NMDAR encephalitis is frequently misdiagnosed as a primary psychiatric disorder, leading to delays in appropriate treatment.2
The pathogenesis of NMDAR encephalitis is driven by autoantibodies directed against the NR1 subunit of the NMDA receptor, resulting in disrupted synaptic transmission and widespread neuroinflammation.1 Standard first-line treatments typically include immunotherapy options such as corticosteroids, plasmapheresis or intravenous immunoglobulin (IVIG), with second-line agents like rituximab or cyclophosphamide considered when necessary. However, treatment responses can vary significantly between individuals. While early and intensive immunotherapy is linked to more favorable neurological outcomes, a considerable proportion of patients continue to struggle with persistent cognitive, psychiatric and functional impairments over the long term.3
Since its identification in 20074, extensive research has focused on characterizing the clinical presentation of the acute phase,5, 6, 7 establishing diagnostic criteria,8, 9 exploring neuroimaging correlates,10, 11, 12, 13, 14 and assessing treatment outcomes.15, 16, 17 While these efforts have significantly advanced our understanding of the disease during its initial stages, research addressing the post-acute phase remains limited.
Although advancements in diagnostic techniques and treatment protocols have improved acute-phase clinical outcomes, the trajectory of recovery from NMDAR encephalitis extends far beyond symptom resolution. Many survivors continue to struggle with cognitive dysfunction, including deficits in working memory, executive function and information processing speed, which impact their ability to return to work, school and daily responsibilities.15 Additionally, persistent psychiatric symptoms, such as anxiety, depression and psychotic episodes, may require ongoing psychiatric care and medication management. The protracted nature of recovery underscores the necessity of comprehensive long-term rehabilitation strategies.
Beyond its direct impact on patients, NMDAR encephalitis profoundly affects caregivers, who frequently undertake extensive responsibilities in supporting patient recovery. Caregivers frequently experience emotional distress, financial strain and social isolation as they navigate the challenges of supporting a loved one with a complex neurological disorder. The unpredictable course of the disease, combined with prolonged hospitalization and the need for continued rehabilitation, places immense psychological, financial and logistical burdens on family members. Many caregivers report experiencing symptoms of chronic stress, burnout, and even post-traumatic stress disorder (PTSD), reflecting the intense emotional toll of witnessing a loved one’s deterioration and uncertain recovery trajectory.16 The evolving caregiving role often requires individuals to become medical advocates, emotional support providers and financial coordinators, all while balancing personal and professional responsibilities.
Despite the crucial role caregivers play in the long-term outcomes of patients with NMDAR encephalitis, their experiences remain significantly underrepresented in the literature.6 Previous research on rare neurological diseases suggests that informal caregivers frequently lack adequate psychological support and face systemic barriers when seeking assistance for themselves or their loved ones.17 The lack of structured caregiver support programs and limited recognition of their needs within healthcare systems further exacerbates these challenges. Also, disparities in healthcare accessibility and inconsistencies in long-term follow-up care contribute to significant variability in patient and caregiver experiences across different healthcare settings.
Research increasingly emphasizes the importance of multidisciplinary approaches to treating NMDAR encephalitis that go beyond acute medical care. Incorporating neuropsychological rehabilitation, caregiver support programs and long-term social reintegration is crucial for improving outcomes for patients and their families.15 The SAPIENCE study addresses these gaps by investigating the long-term burden on caregivers, focusing on their psychological wellbeing, social adaptation and challenges navigating healthcare systems. By highlighting caregivers’ lived experiences, the study aims to inform patient-centered interventions that address the difficulties faced by those caring for individuals with NMDAR encephalitis.
Ultimately, SAPIENCE underscores the need for integrative care models that support both patients and caregivers, promoting a more comprehensive approach to managing the long-term effects of NMDAR encephalitis.
Study overview and methodological framework
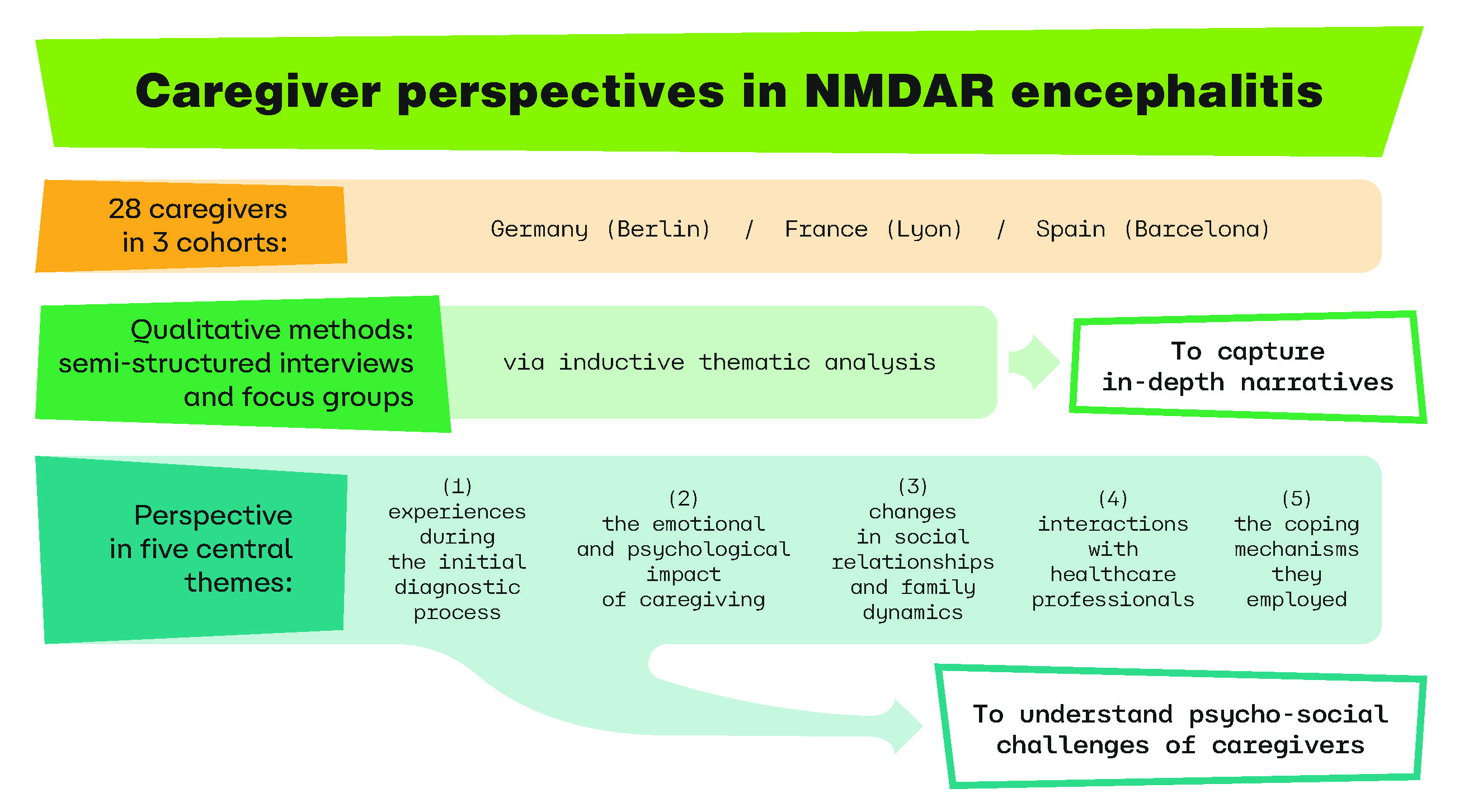
The SAPIENCE study is a multi-center European research initiative designed to evaluate long-term patient and caregiver outcomes. Level 1 participants were recruited from separate cohorts in Germany (Berlin), France (Lyon) and Spain (Barcelona), ensuring broad national representation.
Inclusion required a confirmed NMDAR encephalitis diagnosis,8 age over 17, and fluency in a project language (German, French, Spanish, Catalan, or English). Individuals with preexisting neurological conditions or unable to give informed consent were excluded. The 1st phase of this study employed qualitative methods to capture in-depth narratives from 28 caregivers across 3 European study sites: Barcelona, Berlin and Lyon. Data were collected through semi-structured interviews and focus groups, allowing researchers to uncover recurring themes that shape the caregiving experience. A thorough inductive thematic analysis was conducted on the interview and focus group transcripts, following the methodology outlined by Braun and Clarke. This approach supports the development of themes directly from the data, rooted in participants’ experiences rather than guided by existing theoretical frameworks.18
Caregivers offered valuable perspectives across 5 central themes: 1) their experiences during the initial diagnostic process, 2) the emotional and psychological impact of caregiving, 3) changes in social relationships and family dynamics, 4) interactions with healthcare professionals, and 5) the coping mechanisms they employed. A thematic analysis of these accounts revealed recurring patterns that contribute to a deeper understanding of the challenges encountered by those caring for individuals with NMDAR encephalitis.
Navigating the complexities of diagnosis
Many caregivers described the diagnostic journey as marked by confusion, frustration and emotional distress. Early symptoms often resembled psychiatric disorders, resulting in frequent misdiagnoses and significant delays in receiving appropriate treatment. The prolonged uncertainty surrounding the diagnosis exacerbated caregivers’ emotional burden, often compelling them to advocate continuously for comprehensive neurological evaluations. The lack of prompt clinical recognition of NMDAR encephalitis highlights the urgent need to raise awareness among frontline healthcare professionals.
Emotional and psychological burden
The caregiving role was often marked by intense stress, heightened anxiety and emotional exhaustion. Numerous caregivers described experiencing symptoms similar to PTSD, stemming from the traumatic nature of the illness – witnessing seizures, aggressive behaviors, and enduring lengthy hospital stays. The ongoing demands of caregiving frequently resulted in burnout, highlighting the need for psychological support systems specifically designed for those caring for individuals with neuroimmune disorders.
Vaillant emphasized that extended caregiving responsibilities often necessitate the use of ego defense mechanisms to cope with emotional strain.19, 20 Many caregivers, often unconsciously, relied on strategies such as repression, dissociation and intellectualization to regulate their emotional reactions. Nevertheless, the cumulative psychological impact of caregiving remains substantial, underscoring the importance of structured interventions aimed at addressing both acute and long-term stress experienced by caregivers.
Social impact
Caregivers frequently described significant disruptions to family life, career paths, and personal relationships. The unpredictable course of the illness made it challenging to balance caregiving duties with professional obligations. In many instances, caregivers experienced financial hardship, often as a result of reducing their working hours or having to leave their jobs entirely. Social isolation was also commonly reported, as the intensive demands of caregiving left little time or energy for sustaining social connections or participating in leisure activities.
Coping strategies and resilience
Despite these challenges, caregivers developed various coping mechanisms, including reliance on patient advocacy groups, engagement in mindfulness-based stress reduction techniques and participation in caregiver support networks. Several caregivers emphasized the importance of maintaining a structured routine to manage both their wellbeuing and that of the patient.6 Humor, when appropriate, was cited as a crucial tool in mitigating stress and fostering resilience.
Enhancing holistic support in NMDAR encephalitis care
This qualitative analysis highlights the urgent need for a more holistic approach to managing NMDAR encephalitis – one that actively involves and supports caregivers alongside patients. The considerable emotional, financial and social strain placed on caregivers calls for a shift toward an integrated model of care that prioritizes both patient and caregiver wellbeing. Existing healthcare frameworks tend to focus primarily on acute treatment phases, often neglecting the long-term needs and challenges encountered during recovery. Bridging these gaps will require a comprehensive strategy that includes early intervention, ongoing psychological support, tailored rehabilitation services and broader policy reforms to ensure sustainable, long-term care solutions.
Improved diagnostic training
Early and accurate diagnosis and early treatment remains a fundamental challenge in NMDAR encephalitis management as in chronic diseases with poor prognosis with persistent cognitive impairments. Misdiagnosis or delayed recognition of the disease prolongs patient suffering and exacerbates caregiver stress.2 Standardizing diagnostic protocols, increasing clinician awareness and incorporating NMDAR encephalitis into differential diagnosis training for psychiatrists, neurologists and emergency physicians are essential steps. Furthermore, the integration of biomarkers and imaging advancements, as described by Dalmau et al.,1 may facilitate earlier and more precise detection, reducing the burden of uncertainty on caregivers.
Targeted psychological support
The psychological toll on caregivers is well-documented, with many experiencing symptoms of depression, anxiety and PTSD.5 The unpredictability of patient recovery, coupled with the emotional strain of witnessing severe neuropsychiatric symptoms, necessitates structured mental health interventions. Vaillant highlighted that long-term caregiving responsibilities often require psychological defense mechanisms such as repression and intellectualization, yet these may not be sufficient to mitigate distress.19, 20 Implementing targeted psychological interventions, including structured counseling, peer support groups and stress-reduction programs, can significantly improve caregiver resilience and long-term wellbeing.
Long-term recovery and rehabilitation
While many patients recover from the acute phase of NMDAR encephalitis, persistent cognitive impairments – including deficits in memory, executive functioning, and attention – can hinder full reintegration into daily life.3 These impairments, in turn, increase caregiving demands, often leading to chronic fatigue and emotional exhaustion. Establishing standardized rehabilitation programs, including neuropsychological therapy and cognitive training, can facilitate patient independence and alleviate caregiver burden.
Healthcare system – integrated multidisciplinary care
Fragmented healthcare pathways place considerable strain on caregivers, who often find themselves navigating complex and disjointed systems with little guidance. Participants in this study frequently reported challenges in securing consistent follow-up care and noted a lack of coordination between key healthcare providers, including neurologists, psychiatrists, rehabilitation specialists, and social workers. Establishing integrated multidisciplinary teams – consisting of neurologists, neuropsychiatrists, neuropsychologists, and social workers – can help ensure a more cohesive and continuous care experience, easing the transition from hospital to home. Such collaborative care models, successfully implemented in the management of other chronic neurological conditions, have been shown to enhance long-term patient outcomes while alleviating caregiver burden.17
Enhancing social reintegration strategies
The transition from acute hospitalization to community reintegration is a complex process that affects both patients and caregivers. Many caregivers in this study described challenges in facilitating social re-engagement, particularly for patients experiencing residual psychiatric symptoms or cognitive impairments. Public awareness campaigns, employer education programs, and community-based social integration initiatives can help mitigate stigma and promote a more inclusive environment for individuals recovering from NMDAR encephalitis.17
It is worth to highlight the vital work of patient organizations – such as Encephalitis International, which provides resources, advocacy, and peer support – can further enhance public understanding (https://www.encephalitis.info/about-us/). Notably, initiatives like World Encephalitis Day play a crucial role in raising global awareness and promoting acceptance of those affected by encephalitis.
Limitations
A key strength of this study is its multicenter design, which enabled the inclusion of a diverse sample of patients and caregivers across various healthcare settings and cultural contexts, enhancing the generalizability of the findings. However, the sample size, while sufficient for qualitative analysis, may limit the broader applicability of the results. The analysis is limited to qualitative data without quantitative triangulation. Future project phases will include quantitative methods to validate and expand on these results.
Conclusions
Caregivers of individuals affected by NMDAR encephalitis are essential contributors to the recovery process, yet their roles and challenges often go unrecognized in clinical practice and health policy. The SAPIENCE study underscores the urgent need to address the multifaceted obstacles they encounter – ranging from diagnostic delays and psychological strain to gaps in rehabilitation services and systemic support. These findings emphasize the importance of developing comprehensive, integrated care models that prioritize the wellbeing of both patients and their caregivers. Future research should focus on creating and evaluating targeted interventions for caregivers, paving the way for more inclusive, patient- and caregiver-centered healthcare systems. Our findings align with the most recent World Health Organization (WHO) Technical Brief on Encephalities, which emphasizes that individuals recovering from encephalitis often require long-term care, placing significant emotional, financial and social burdens on caregivers.21
Use of AI and AI-assisted technologies
Not applicable.