Abstract
Heart failure with preserved ejection fraction (HFpEF) poses a significant clinical challenge due to its increasing incidence, diagnostic complexities and pathophysiological heterogeneity. This study offers valuable insights into the role of urinary biomarkers in patients with HFpEF. Our research focused on profiling alterations in urinary biomarkers, encompassing albumin, indicators of tubular injury, oxidative stress markers, and proteomic changes in individuals with this condition. These findings may provide a potential tool for addressing the diagnostic challenges associated with HFpEF, particularly given the absence of specific cutoff points in the diagnosis of this disease. Furthermore, we explored the potential pathophysiological relationships of these biomarkers, which, in a broader context, facilitate a deeper understanding of this complex disease and may identify potential pharmacotherapeutic targets. We also examined the prognostic value of the identified biomarkers, which could serve as useful instruments for predicting disease risk and forecasting clinical outcomes. Additionally, we emphasized the existing knowledge surrounding potential biomarkers, suggesting that a better understanding of these markers may contribute to the development of clinically relevant tools and enhance our comprehension of HFpEF. The findings from this study align with the current literature, which underscores the complexity of HFpEF and the need for innovative diagnostic, prognostic and therapeutic strategies.
Key words: diastolic dysfunction, albuminuria, HFpEF, heart failure with preserved ejection fraction, urinary biomarker
Introduction
Heart failure with preserved ejection fraction (HFpEF) is a heterogeneous condition posing significant medical and societal challenges. Its prevalence is estimated to be approx. 1–2% in adults, rising to about 5% in those over 60 years.1, 2 These figures may be underestimated due to insufficient recognition of the condition.3 The incidence of HFpEF is projected to rise with aging populations and the growing prevalence of lifestyle-related diseases, such as hypertension, diabetes and hyperlipidemia, which contribute to the pathogenesis of HFpEF. Research in HFpEF is becoming crucial for improving patients’ quality of life and treatment outcomes.
Diagnosing HFpEF is challenging in clinical practice due to the absence of a definitive biochemical or echocardiographic marker. The mere presence of diastolic dysfunction is insufficient for establishing a diagnosis of HFpEF. Many diagnostic parameters lack clear cutoffs, and symptoms appear only during physical exertion, requiring exercise testing for accurate diagnosis. Although invasive hemodynamic testing is regarded as the reference standard, its use is limited by its benefit–risk ratio and the substantial number of suspected cases.4 The lack of a universally accepted diagnostic guideline leads to many HFpEF patients being misdiagnosed or inadequately diagnosed in the early stages, often until the disease has progressed significantly.
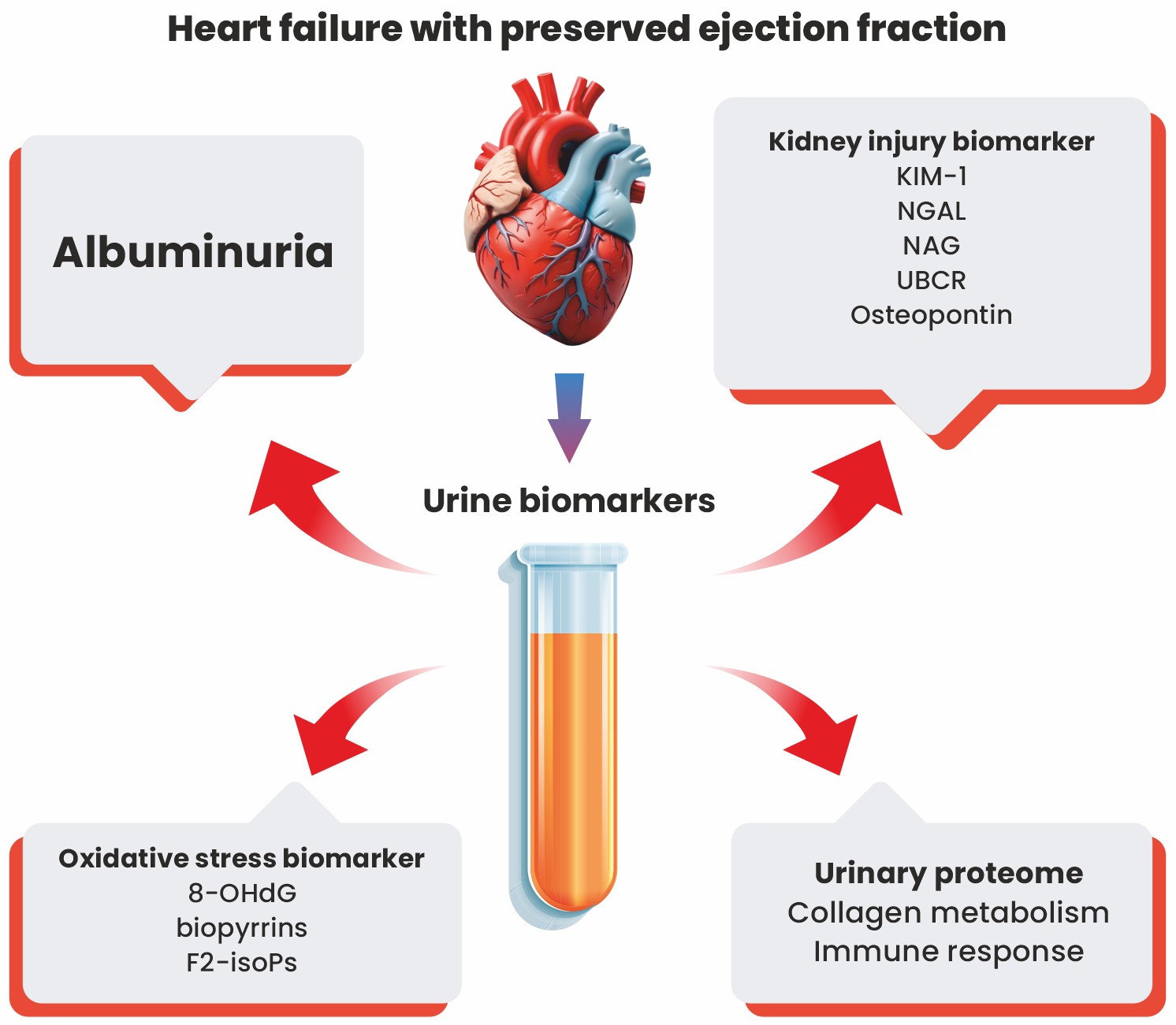
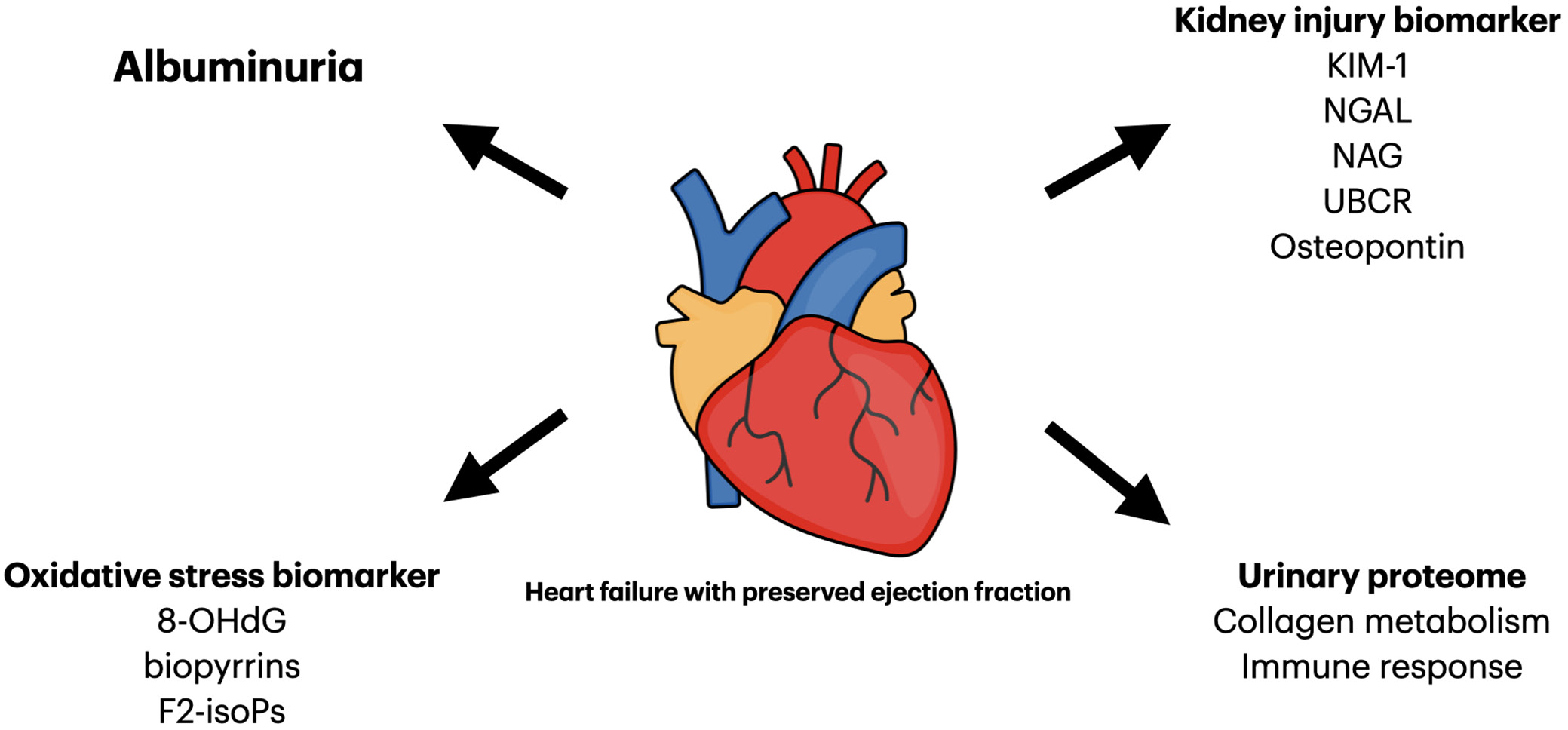
The classification of HFpEF highlights its distinct pathophysiology compared to heart failure with reduced ejection fraction (HFrEF). Key components of HFpEF pathophysiology include systemic inflammation, increased oxidative stress and endothelial dysfunction, leading to structural cardiac remodeling and its subsequent effects.5 Despite extensive research, these processes remain incompletely understood. This review summarizes current knowledge on urinary biomarkers in patients with HFpEF, evaluating their diagnostic and prognostic value while contributing to a better understanding of the pathophysiology of this complex clinical entity (see Figure 1 and Table 1).
Objectives
This review consolidates current knowledge on urinary biomarkers in HFpEF patients, focusing on those specific to HFpEF rather than general heart failure (HF). Our study identifies both well-known biomarkers and highlights potential biomarkers that require further investigation. Understanding these biomarkers may shed light on the pathophysiological processes in patients diagnosed with HFpEF. Since these biomarkers are accessible through noninvasive urine collection, they provide valuable insights into the underlying pathology. This knowledge could facilitate the identification of new therapeutic targets and optimize the patient care. Urinary biomarkers may also serve as diagnostic tools, identifying individuals at risk of developing HFpEF or aiding its diagnosis. Additionally, this review examines the evidence for their predictive value in patients with HFpEF.
We conducted a comprehensive PubMed search from July 2023 to June 2024, using specific key words and relevant subheadings. The key words included: “heart failure with preserved ejection fraction urinary biomarker”, “heart failure with preserved ejection fraction albuminuria”, “HFpEF urinary biomarker”, “diastolic dysfunction urinary biomarker”, “diastolic dysfunction albuminuria”, “heart failure with preserved ejection fraction NGAL”, and “heart failure with preserved ejection fraction KIM-1”. Results were combined, duplicates removed, and articles assessed for relevance based on titles, abstracts or full texts. Only English-language articles directly related to the topic were included, regardless of publication date. Studies involving animals were excluded.
Albuminuria
In physiological states, the glomerular barrier prevents filtration of large proteins, such as albumin, through size- and charge-selective membrane. The negatively charged endothelial membrane with its fenestrations restricts the filtration of negatively charged albumin in the renal glomerulus.6 This results in albumin concentrations in the ultrafiltrate within Bowman’s space being 1000–10,000 times lower than in plasma. Most albumin molecules that pass through are absorbed by proximal tubule cells, where proteases break them down into fragments that can re-enter the urine. Elevated levels of albumin in urine are a recognized symptom of glomerular endothelial damage. Moreover, the population-based Maastricht Study demonstrated a direct relationship between albuminuria and microvascular endothelial dysfunction.7 A significant correlation was observed between 24-h albuminuria and 2 established measures of microvascular endothelial function: retinal arteriolar dilation in response to flicker light stimulation and skin hyperemia induced by local heating. The presence of albuminuria also carries broader implications for systemic health. Transient albuminuria can occur in response to high-altitude hypoxia, myocardial hypoxia and physical exertion, whereas its persistent presence is commonly associated with metabolic syndrome, type 2 diabetes and cardiovascular diseases.8
Albuminuria is a major risk factor for cardiovascular and overall mortality, independent of other cardiovascular risk factors, even in individuals with normal renal function.9 An elevated urinary albumin-to-creatinine ratio (UACR) is common among patients with HF, and this association remains significant even in individuals without diabetes.10 Moreover, it has been shown that low-grade albuminuria precedes the occurrence of both HFpEF and HFrEF.11 According to these findings, elevated albuminuria indicates systemic vascular endothelial dysfunction and is pathophysiologically linked to HF, including HFpEF.12 The association between albuminuria and HFpEF was demonstrated in the prospective multicenter PROMIS-HFpEF study.13 It identified a link between albuminuria and coronary microvascular dysfunction, as well as systemic endothelial dysfunction, evidenced by elevated UACR and reduced coronary flow reserve. These dysfunctions correlated with markers of systemic endothelial dysfunction, including UACR. Therefore, albuminuria serves as an indicator of widespread microvascular and endothelial damage and may act as a surrogate marker for such pathological changes in multiple organs, including the heart. However, the precise pathomechanisms and causal link between albuminuria and HF remain unclear, although inflammation-induced endothelial dysfunction is considered a potential contributing factor.13 In the RELAX study, 75% of patients with HFpEF exhibited elevated levels of C-reactive protein (CRP).14 Correlations were observed between inflammatory markers, such as von Willebrand factor, in patients with both albuminuria and HF, with this factor further associated with increased levels of interleukin 6 (IL-6) and CRP.15 Another marker supporting the link between inflammation and the pathophysiology of HFpEF is pentraxin 3 (PTX-3), a novel inflammatory biomarker. Its levels have been shown to correlate with the presence of left ventricular diastolic dysfunction in patients with preserved ejection fraction.16 Moreover, elevated levels of PTX-3) have also been associated with diastolic remodeling in patients experiencing ST-elevation myocardial infarction (STEMI).17
Furthermore, hypervolemia is another potential mechanism linking albuminuria to HFpEF. Studies have confirmed associations between albuminuria and reduced renal artery blood flow, as well as physical signs of volume overload and elevated levels of NT-proBNP.18 Additionally, according to this hypothesis, a reduction in albuminuria has been associated with an improvement in congestion-related symptoms, as well as a decrease in NT-proBNP levels.19
Albuminuria is also associated with echocardiographic parameters reflecting biventricular dysfunction and myocardial remodeling.20 This relationship persisted even after excluding comorbid conditions such as diabetes and chronic kidney disease (CKD), and correlations with changes in echocardiographic parameters have been observed even at low levels of albuminuria in asymptomatic patients. Studies have shown that albuminuria is associated with increased left ventricular (LV) mass (LVM) and wall thickness in both hypertensive and non-hypertensive individuals.21, 22, 23 In hypertensive patients, it correlates negatively with ejection fraction and left LV chamber size.21 Renal impairment also affects left heart geometry; however, the specific alterations in cardiac structure and function vary depending on whether albuminuria or a reduced estimated glomerular filtration rate (eGFR) is present.24 In patients with albuminuria but normal creatinine levels, eccentric hypertrophy is more common, while isolated reductions in eGFR are linked to concentric hypertrophy, increased LV mass and abnormal LV geometry alongside lower mid-wall fractional shortening (MWFS). Patients with both albuminuria and reduced eGFR exhibit mixed structural changes, including eccentric and concentric hypertrophy, as well as concentric remodeling.24 The above observations suggest that albuminuria and eGFR are associated with different pathomechanisms leading to HFpEF. This also indicates the potential to identify subgroups of patients with diastolic dysfunction in future studies.
Higher UACR levels are linked to worse LV systolic function parameters, such as longitudinal systolic function (measured by tissue Doppler’s velocity) and preload recruitable stroke work (PRSW, a load-independent indicator of contractility), despite the presence of preserved ejection fraction.20, 25 Global longitudinal strain (GLS), a sensitive echocardiographic parameter, is crucial for assessing subtle changes in LV systolic function in patients with HFpEF.26 Studies indicate that HFpEF patients often exhibit abnormalities in GLS, suggesting underlying systolic dysfunction, which may be an inherent part of the HFpEF syndrome.26, 27, 28 Notably, UACR exhibits an inverse relationship with GLS, and this association remains significant even after adjustment for multiple confounding variables. Another parameter indicative of LV diastolic relaxation is the e′ tissue velocity, which reflects the diastolic motion of the myocardium during the rapid filling phase of the ventricle.29 While some studies have reported an association between albuminuria and reduced e′ velocity, the strength and significance of this relationship have varied across different analyses.25, 30 Nonetheless, albuminuria, even at low concentrations, consistently correlates with an elevated E/e′ ratio.25 The E/e′ ratio is regarded as one of the most reliable noninvasive measures for assessing LV filling pressure in individuals with preserved diastolic function. Importantly, this relationship persists after accounting for diabetes and LV hypertrophy, indicating a subclinical connection between albuminuria and deteriorating function. Additionally, an analysis of B-type natriuretic peptide (BNP) levels and UACR in patients with preserved ejection fraction and normal LV volume revealed a strong positive correlation.25 This suggests that elevated albuminuria may serve as a biomarker for heightened myocardial wall stress, a key contributor to HFpEF pathophysiology.
In patients with HFpEF, right ventricular dysfunction is common and associated with worse clinical outcomes in this population. Furthermore, research findings indicate that longitudinal subendocardial dysfunction, both diastolic and systolic, of the right ventricle is related to the symptomatology of patients.20 Albuminuria is significantly associated with right ventricular (RV) remodeling. Structural changes such as increased RV wall thickness and chamber enlargement are frequently observed in patients with HFpEF.20 The urinary albumin-to-creatinine ratio is significantly elevated in individuals with RV hypertrophy, and higher levels are correlated with increased RV wall thickness and a larger RV end-systolic area index. Furthermore, albuminuria is associated with RV systolic dysfunction, as indicated by reduced right ventricular fractional area change (RVFAC). These associations persist even after excluding patients with macroalbuminuria, and they remain significant after adjusting for increased pressures in the right heart, such as pulmonary artery systolic pressure (PASP) and right atrial pressure (RAP), as well as left ventricular diastolic pressure measured via catheterization. This suggests that albuminuria-related RV remodeling may result from mechanisms beyond preload or afterload increases, possibly involving inflammation and endothelial dysfunction.
In clinical terms, albuminuria emerges as a promising biomarker for HFpEF onset, as traditional cardiovascular biomarkers exhibit a stronger correlation with HFrEF. Low-grade albuminuria preceding HFpEF suggests its potential as an early indicator of cardiovascular pathology.11 Studies have shown that elevated UACR is associated with a higher risk of hospitalization in HFpEF patients, an effect that is notably stronger in males.31 In individuals with HFpEF, urinary albumin excretion has also been identified as an independent predictor of both cardiovascular and non-cardiovascular mortality across all eGFR levels.32 Moreover, positive findings of albuminuria on urine dipstick tests in HFpEF patients have also been associated with poorer outcomes.33, 34 This evidence suggests that dipstick albuminuria could serve as a simple yet effective prognostic marker in HFpEF patients, enabling early risk stratification and guiding clinical management.
Tubular kidney injury biomarkers
Tubular kidney injury biomarkers are emerging as valuable tools for the early detection and evaluation of kidney damage. Unlike traditional markers such as serum creatinine, which often reflect kidney injury only after significant delays, tubular injury biomarkers can detect damage at earlier stages, allowing for differentiation of the site and degree of kidney injury.35
Kidney injury molecule-1 (KIM-1) is a type I cell membrane glycoprotein that is undetectable in healthy kidneys. However, in response to inflammation or injury of the proximal tubules, it is expressed in regenerating epithelial cells.36 This upregulated expression is particularly prominent in the S3 segment of the proximal tubule, where KIM-1 functions as a scavenger receptor, facilitating the phagocytosis of necrotic epithelial cells.37 In patients with chronic HF, elevated levels of KIM-1 in the urine correlate with worse clinical outcomes and increased risk of hospitalization.38 Additionally, elevated KIM-1 levels are observed in symptomatic HF patients.38 These elevations persist even in patients with normal kidney function and normal glomerular filtration rate (GFR). Furthermore, elevated levels of KIM-1 in urine are correlated with an increased risk of developing HF within the population.39 Comparing the urinary marker profile in patients with HFrEF versus HFpEF, patients with diastolic dysfunction show greater evidence of tubular damage and/or dysfunction.40 Among HFpEF patients, higher urinary KIM-1 levels are noted, while urinary creatinine levels are significantly lower compared to those with HFrEF.40 Additionally, pediatric studies have linked elevated urinary KIM-1 concentrations to left ventricular hypertrophy (LVH), the most common myocardial structural abnormality in diastolic dysfunction.41
Another biomarker, neutrophil gelatinase-associated lipocalin (NGAL), is typically present at low levels in healthy individuals but rises markedly in response to kidney injury. It serves roles in innate immunity and acts as an acute-phase protein in inflammatory states and endothelial damage.42 Its heightened concentration in urine stems from increased protein expression and impaired reabsorption in damaged proximal tubule epithelium.42 Research has shown that NGAL levels in both serum and urine are significantly increased in outpatients with HF, suggesting its potential utility as a diagnostic and prognostic indicator in this condition.43, 44 This correlation remained significant in patients with reduced GFR. Interestingly, while serum NGAL levels are correlated with serum creatinine in acute HF,45 urinary NGAL concentrations do not show this association. The data on the predictive value of urinary NGAL levels in predicting mortality in patients with chronic HF are inconclusive, with only 1 study demonstrating a weak correlation with elevated mortality in this patient cohort.43, 44, 46 However, similarly to KIM-1, the study shows that patients with HFpEF exhibit higher urinary NGAL-1 levels compared to patients with reduced ejection fraction, particularly when there is no kidney dysfunction.40 Furthermore, in patients with CKD, plasma NGAL concentration correlated with LVH and left ventricular diastolic dysfunction, as assessed by the E’ parameter and the ratio of E to E’ (E/E’).47
Going further, N-acetyl-β-D-glucosaminidase (NAG), a lysosomal enzyme released from proximal tubules due to epithelial cell injury, is significantly elevated in patients with chronic HF.48 Its levels correlate with poorer prognosis and increased risk of hospitalization.37, 46, 48 However, no clear relationship has been established between NAG levels and HF-related events in HFpEF, defined as hospitalization or death due to HF. In contrast, a study showed that the urinary β2-microglobulin to creatinine ratio (UBCR) indicated a significantly higher risk of cardiac events in patients with HFpEF, and this association persisted even after adjusting for other risk factors.49 Levels of UBCR also correlate with HF severity, as classified by the New York Heart Association (NYHA) functional classification, in patients with HFpEF.49 Another biomarker found in urine that shows significantly elevated levels in patients with HFpEF is osteopontin,40 a protein secreted by cells in the distal tubule and loop of Henle in response to nephron injury. While its role in diastolic dysfunction remains unclear, further investigation is warranted.
The observed relationships between HFpEF and tubular kidney injury biomarkers highlight the need for deeper investigation into the underlying mechanisms. These biomarkers likely reflect the functional status of the renal tubules, which are responsible for electrolyte and water balance. A study conducted by Jungbauer et al. revealed that alterations in volume status induced by diuretics are linked to changes in markers of tubular dysfunction, such as KIM-1 and NGAL.38 Disruption in salt and water excretion can result in fluid overload, and therefore elevated cardiac output, high blood pressure, LVH, and indirectly contribute to HFpEF development. Tubular injury, reduced nephron mass and ongoing inflammation may activate both the renin–angiotensin–aldosterone system and the sympathetic nervous system, causing endothelial dysfunction.50 Moreover, the referenced studies observed higher concentrations of tubular injury biomarkers in patients with HFpEF compared to those with HFrEF, particularly in cases with normal eGFR.40 This suggests that renal dysfunction may be present in HFpEF patients without diagnosed kidney disease, as eGFR primarily assesses kidney filtration capacity and may not accurately reflect existing damage in the distal nephron segments. Proximal tubules, which are highly susceptible to injury due to their substantial oxygen demand, play a central role in the progression of CKD. In turn, CKD is associated with the accumulation of uremic toxins, increased oxidative stress and microvascular dysfunction, i.e., key contributors to the development and progression of diastolic heart dysfunction.51, 52 While current data strongly suggest a connection between HFpEF and tubular injury biomarkers, causality remains unproven. Reverse causation, where HFpEF contributes to tubular injury, must also be considered.
Oxidative stress markers
In the literature on the HFpEF pathophysiology, oxidative stress, along with endothelial dysfunction and inflammation, plays a significant role in the development of diastolic dysfunction of the heart.52 Oxidative stress arises from an imbalance between excessive production of reactive oxygen species (ROS) and insufficient antioxidant defenses, leading to cellular damage that affects proteins, lipids and DNA. Patients with HFpEF frequently present with comorbidities such as obesity, diabetes, dyslipidemia, hypertension, and renal impairment, all of which contribute to endothelial dysfunction and systemic inflammation, thereby enhancing ROS production in cardiac endothelial cells.53 Moreover, studies have shown that the presence of HFpEF correlates with elevated levels of oxidative stress markers, such as nitrotyrosine, indicating nitrosative/oxidative stress.54 Reactive oxygen species can alter titin phosphorylation, leading to increased passive stiffness of cardiomyocytes, which may adversely affect cardiac diastolic function.55 Additionally, ROS-induced secretion of pro-fibrotic substances promotes myofibroblast differentiation and collagen deposition, contributing to cardiac fibrosis.56 Mitochondrial structural and functional disruption in cardiomyocytes, another consequence of oxidative stress, is strongly implicated in the pathophysiology of HFpEF.57
One of the well-established biomarkers of oxidative stress is 8-hydroxy-2′-deoxyguanosine (8-OHdG), also known as 8-oxo-2′-deoxyguanosine (8-oxo-dG). It is generated as one of the main products of DNA oxidation by ROS. Formed from the oxidation of deoxyguanosine within DNA, 8-OHdG is repaired and removed by 8-oxoguanine DNA glycosylase-1, then transported into the bloodstream, filtered by the kidneys and excreted in urine.58 Elevated 8-OHdG levels in serum and urine reflect systemic oxidative stress. In the conducted meta-analysis of studies focusing on 8-OHdG in patients with HF, a strong positive correlation has been demonstrated.59 Furthermore, in studies of patients with HF, it has also not been shown that diabetes affects the concentration of the biomarker. Urinary 8-OHdG levels have been shown to correlate with HF symptom severity, as assessed using the NYHA functional classification, as well as with echocardiographic parameters including left ventricular ejection fraction (LVEF), pulmonary capillary wedge pressure, and left ventricular end-diastolic volume index (LVEDVI).60 Laboratory markers like BNP60 also show significant associations. Urinary 8-OHdG has emerged as an independent prognostic marker for cardiac events in patients with chronic HF.61 Furthermore, in asymptomatic individuals with hypertension, increased urinary 8-OHdG levels correlate with subclinical diastolic dysfunction. In the cohort of individuals without diagnosed HF but with arterial hypertension, the association between 8-OHdG levels and cardiac function has been evaluated. The investigation revealed that parameters of diastolic dysfunction, such as mitral annular early diastolic velocity (e’) and the ratio of early transmitral flow velocity (E) to e’ (E/e’), correlated with increased urinary 8-OHdG excretion.62
Biopyrrins, formed through the oxidative metabolism of bilirubin, serve as additional biomarkers of oxidative stress and can be detected in the blood and urine. Bilirubin, an antioxidant, captures circulating ROS to prevent lipid and low-density lipoprotein (LDL) oxidation. However, this process is self-limiting, and biopyrrins are subsequently excreted in urine, making them a noninvasive biomarker.63 In a study conducted by Hokomaki et al., urinary biopyrrins concentrations are significantly elevated in patients with HF, with the highest levels observed in patients classified as NYHA III/IV.64 Even in patients with milder symptoms (NYHA I) and preserved ejection fraction (average 54.8 ±2.7%), biopyrrin levels are significantly higher than in controls. A positive correlation has been observed between biopyrrin and BNP levels.64 Further research has focused on bilirubin levels, which are associated with poorer prognosis, increased severity in patients with HF and elevated all-cause mortality.65, 66 However, in patients with HFpEF, lower blood bilirubin levels have been observed compared to control subjects, and this decrease correlates with the severity of diastolic dysfunction, with the lowest levels detected in those with grade 4 HFpEF.67 This discrepancy in study results depending on the type of HF may be explained by the role of bilirubin as an antioxidant,68 which may decrease in HFpEF due to increased oxidative stress. Regarding biopyrrins, it has been shown that their concentration in urine correlates with bilirubin levels.69 Therefore, it seems reasonable to hypothesize about the potential value of biopyrrins as a biomarker in HFpEF. However, further studies are required to establish their clinical utility in specific HF subtypes.
Another potential biomarkers of oxidative stress in HFpEF measurable in urine are F2-isoprostanes (F2-isoPs). These compounds are advantageous due to the non-invasive nature of their assessment and their stability, as their concentrations are not significantly influenced by renal or hepatic dysfunction. Furthermore, F2-isoPs are considered one of the most reliable and stable markers for monitoring oxidative stress intensity in patients.70 Research indicates that the concentration of F2-isoPs in urine is significantly elevated in patients with severe HF and correlates with the severity of symptoms as indicated by the NYHA scale.70 Although promising, additional studies are needed to determine the predictive value of F2-isoPs and their specific relationship to HFpEF.
Urinary proteome
Urinary proteome analysis is an evolving field in biomarker discovery, offering insights into naturally occurring peptides in urine. This approach has become a valuable tool for understanding disease mechanisms and identifying novel biomarkers across various conditions. Heart failure, including HFpEF, presents a multifactorial etiology, making it challenging to unravel the precise molecular mechanisms involved. In all HF subtypes, including HFpEF, the strongest correlations have been observed with peptides representing collagen fragments, whose concentrations in urine have decreased.71 The most pronounced reductions are observed in fragments derived from collagens with specialized structures that support network formation, particularly collagen types IV and VIII. While the exact cause of these changes is unclear, these findings suggest enhanced collagen network stability in HF and underscore the role of disrupted collagen turnover in patients with HFpEF.72 Further alterations observed in the urinary proteome of patients with HF includes dysregulation in pathways responsible for immune response. The most prominent alterations are associated with innate immune responses, notably those involving toll-like receptors (TLRs), neutrophil degranulation and activation of the complement cascade.71 Notably, these changes are characteristic of HF and remain distinct from those caused by CKD. Despite significant differences between patients with HF and the control group, no significant differences in peptide changes have been observed between patients with reduced and preserved ejection fraction. These findings may indicate that, irrespective of clinical distinctions, HFpEF and other HF subtypes involve overlapping molecular mechanisms. An analysis of data from the TOPCAT study was conducted to assess the prognostic value of urinary proteins in patients with HFpEF. The findings revealed that more than 40 urinary peptides were significantly associated with adverse outcomes, defined as an increased risk of mortality or hospital readmission. The proteins associated with the highest risk included angiopoietin-like protein 2 (ANGPTL2), deoxyribonuclease-1 (DNASE1) and α-amylase 2A (AMY2A). A weaker correlation was observed for proteins related to fibrosis, metabolism and inflammation. In this context, the findings align with other research indicating that urinary biomarkers can provide valuable insights into the prognosis of HFpEF patients.73
Conclusions
Urinary biomarkers show considerable potential as valuable instruments for the diagnosis, prognosis and elucidation of the pathophysiological mechanisms underlying HFpEF. This review consolidates current knowledge on urinary biomarkers, highlighting their utility in advancing the understanding of HFpEF and guiding future research. Given the substantial heterogeneity of HFpEF, it continues to pose a major clinical challenge. Further investigations are crucial to refine the understanding of biomarkers in HFpEF patients, paving the way for improved management and therapeutic strategies for these patients.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.