Abstract
Background. Out-of-hospital cardiac arrests (OHCA) are a major global health concern, occurring frequently worldwide. Obesity may impact outcomes in OHCA patients.
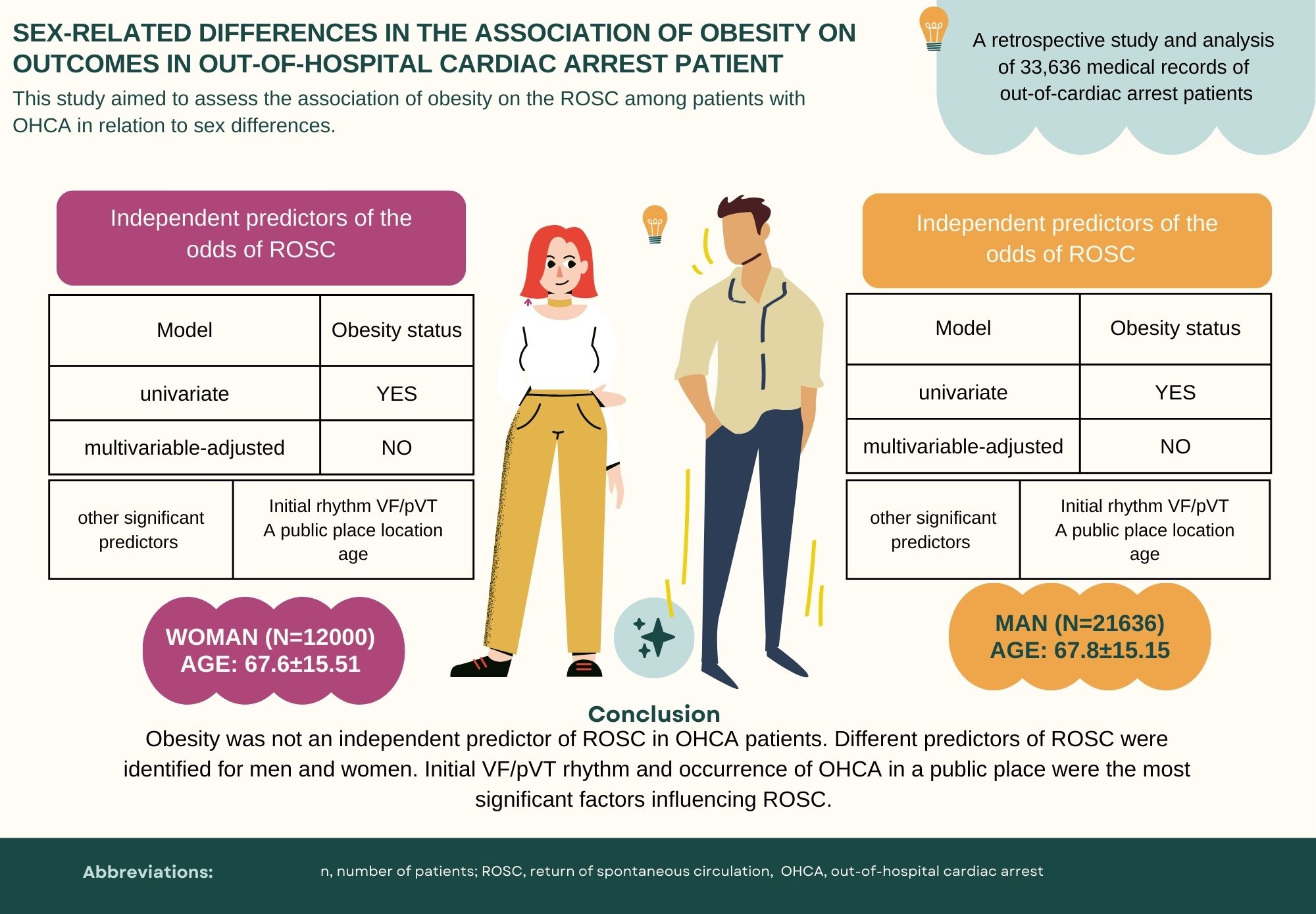
Objectives. This study aimed to assess the impact of obesity on the return of spontaneous circulation (ROSC) in OHCA patients, considering sex differences.
Material and methods. A retrospective cohort study was conducted, analyzing medical records of patients assisted by the Emergency Medical System (EMS) in Poland from January 2021 to June 2022. The study included 33,636 patients with OHCA. Obesity status was determined using ICD-10 codes (E66) and descriptive diagnoses recorded by EMS teams.
Results. Univariate analysis indicated that obesity decreased the odds of ROSC by 25.47% (odds ratio (OR) = 0.75, 95% confidence interval (95% CI): 0.61–0.92) in women and by 19.76% (OR = 0.80, 95% CI: 0.66–0.97) in men. However, multivariate analysis, adjusting for confounding variables, did not confirm a statistically significant impact of obesity on ROSC outcomes. The likelihood of ROSC was significantly higher in individuals with an initial ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) rhythm compared to Asystole/pulseless electrical activity (PEA), being 4.204 times higher in women (95% CI: 3.525–5.014) and 3.655 times in men (95% CI: 3.320–4.023). Out-of-hospital cardiac arrest in a public place increased the odds of ROSC more than twofold for both sexes (women: OR = 2.20, 95% CI: 2.00–2.43; men: OR = 2.13, 95% CI: 1.98–2.29). Among women without obesity, hypertension decreased the odds of ROSC by 11.11% (OR = 0.89, 95% CI: 0.81–0.99).
Conclusions. Our study demonstrated that obesity was not an independent predictor of ROSC in OHCA patients. Different predictors of ROSC were identified for men and women. Initial VF/pVT rhythm, location of OHCA and age were the significant factors influencing ROSC.
Key words: obesity, cardiopulmonary resuscitation, OHCA, ROSC
Background
Out-of-hospital cardiac arrests (OHCA) are a significant global health issue, with an average incidence of 55 cases per 100,000 people annually.1, 2 It is estimated that there are between 300,000 and 700,000 cases each year in the European Union, with a survival rate of 8–10%.2, 3, 4 These situations, which occur suddenly and unexpectedly, are associated with a high risk of mortality and severe neurological failure.5, 6 In Spain, there are approx. 30,000 cases of OHCA annually, resulting in around 20,000 deaths. In Poland, there are approx. 64,000 cases of OHCA annually, with a survival rate close to 20%.7, 8, 9 Although the return of spontaneous circulation (ROSC) occurs in 10–50% of patients with OHCA after starting advanced life support (ALS), mortality rates remain very high. According to the European Resuscitation Council (ERC), OHCA results in approx. 275,000 deaths annually in Europe.9 Other factors influence the survival of these patients, such as the place of occurrence of the event, the presence or absence of obesity, or their sex.3, 10, 11
We are faced with another global public health problem, obesity. This disease affects up to 53% of the European population and 42% of Americans.3, 12, 13, 14 An abnormal body mass index (BMI), which is more prevalent among women than in men,15, 16 is a factor that worsens the prognosis of patients with OHCA. This is due to the pathophysiology of the disease itself and the increased risk of cardiovascular events such as hypertension (HT), coronary events or heart failure (HF), as well as the difficulty when performing chest compressions.3, 5, 12 Although acute coronary syndrome (ACS) is the leading cause of OHCA and obesity is a recognized risk factor for ACS, studies such as those by Tanaka et al. and Berdowski et al. confirm these associations but do not account for sex differences.1, 17
The scientific literature agrees that there are differences in the diagnosis and treatment of cardiovascular events according to sex, with women who suffer OHCA having more unfavorable prognostic factors3, 17, 18 and fewer probability of overall survival and survival with a good neurological condition.19, 20 In general, we observed an underdiagnosis of cardiovascular risk in women,20, 21 with this sex being the most affected by cardiovascular diseases (CVD).18, 20, 22 On the one hand, studies show that women have a greater probability of experiencing OHCA in the absence of witnesses because women tend to spend more time alone or at home since they have a greater life expectancy than men and are more likely to be widowed.19, 20, 22, 23, 24 These factors cause a delay in cardiopulmonary resuscitation (CPR) of patients, which gives them lower survival rates. On the other hand, there is evidence that the factors associated with CVD (diabetes, obesity, psychological stress) are more prevalent in the female sex, which gives them a greater cardiovascular risk.19, 20, 21 Additionally, fewer women compared to men have been observed in CVD research studies, and specific guidelines for women are often based on studies of men, resulting in lower diagnostic ability and delayed treatment and detection of the disease.18, 25, 26, 27
While earlier studies suggested an “obesity paradox” where higher BMI was associated with better outcomes in OHCA patients,28, 29 more recent studies have debunked this theory, indicating that obesity is not a protective factor.30, 31 Recent findings highlight that this paradox might be more accurately described as a “BMI paradox”, as greater adiposity, when measured using alternative anthropometric indices, is associated with worse outcomes.32, 33 It is of great importance to determine which patient conditions can aggravate or improve the chance of ROSC, some of them being modifiable factors (such as obesity, comorbidities and the time between OHCA and CPR initiation) or non-modifiable factors (such as age, sex or initial heart rhythm).8, 30
Other factors can also intervene in the prognosis of patients with OHCA, such as the initial rhythm of ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) or their age and sex.3, 5, 28 It is of great importance to determine which patient conditions can aggravate or improve the chance of ROSC, some of them being modifiable factors (obesity or comorbidities) or not (age, sex or initial heart rhythm).
Patients experiencing OHCA with a shockable rhythm have been shown to have a higher rate of survival and recovery. This is attributed to the higher ROSC rate achieved through the application of an external defibrillator, which significantly increases the likelihood of ROSC.6, 17, 34 Differences in the prevalence and diagnosis of cardiovascular events and obesity in women indicate the need to adopt new approaches to address the sex difference in the treatment of patients with OHCA. In the general population, younger women have a lower prevalence of CVD compared to men. However, women who experience OHCA are typically post-menopausal, with higher rates of obesity and consequently a higher prevalence of CVD compared to men. These 2 factors significantly influence both the cause and subsequent survival of patients.13, 15, 20, 22 No scientific literature has been found that addresses these differences, so we believe it is important to study them to perform an individualized evaluation of patients with OHCA. In our previous study (in which we did not disaggregate patients by gender), obesity results were an independent factor that decreased the odds of ROSC by more than 8%.5 Given the lack of literature and the results of our previous research, we decided to investigate sex differences in this area.
Objectives
This study aimed to assess the association of obesity on the ROSC among patients with OHCA in relation to sex differences.
Methods
Study design and setting
A retrospective cohort study was conducted, involving an analysis of medical records for patients assisted by the Emergency Medical System (EMS) in Poland from January 2021 to June 2022. For this study, data were obtained from the Command Support System of the National Emergency Medical Service. The dataset included all documented cases of OHCA with International Classification of Diseases (ICD-10) code I46, where CPR was initiated. In Poland, there are 2 types of emergency medical teams (EMTs). Specialized EMTs (S-EMTs) comprise at least 3 persons, including a physician and an emergency nurse or paramedic. Basic EMTs (B-EMTs) comprise at least 2 persons qualified to perform medical emergency activities, including an emergency nurse or paramedic. As of the 1st half of 2023, there were 1,600 EMTs in Poland, including 1,284 B-EMTs and 316 S-EMTs.
Study population
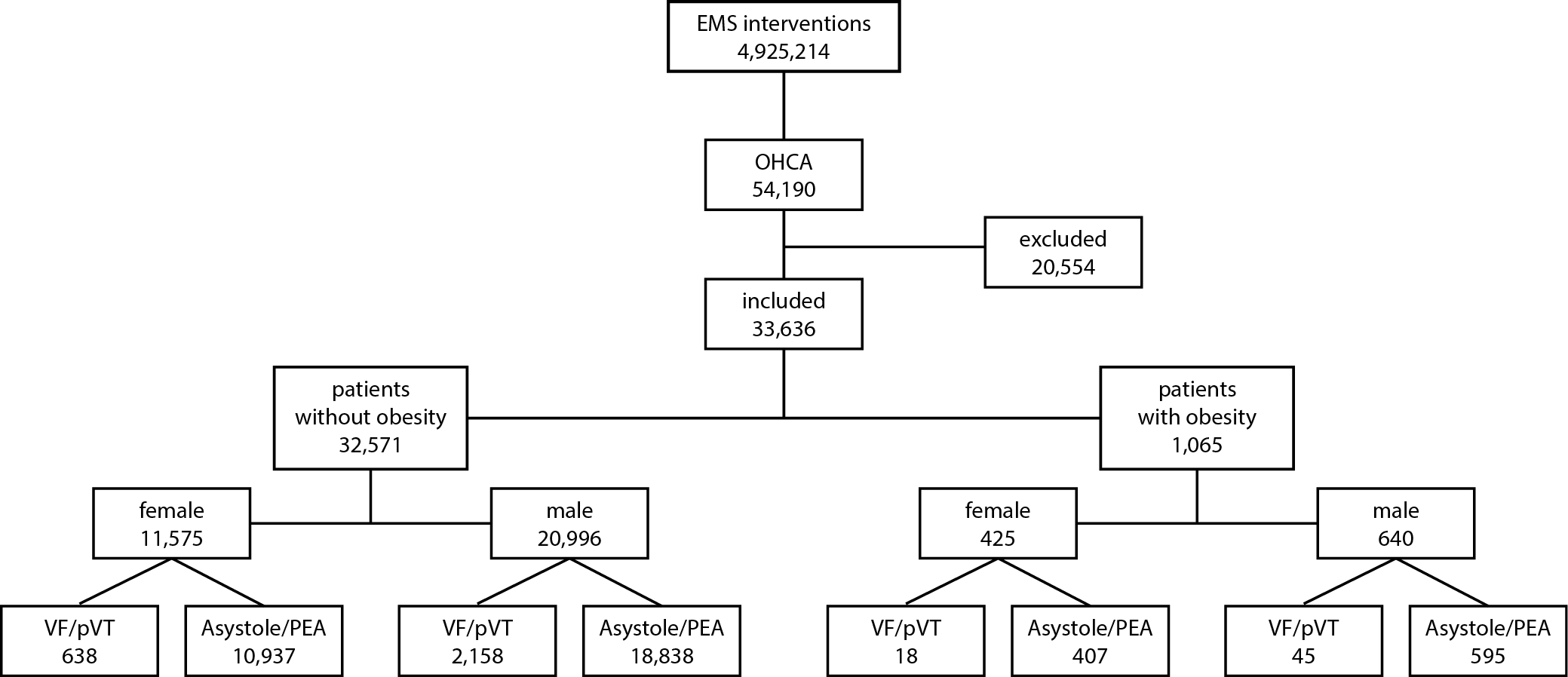
A total of 4,925,214 EMS records were analyzed. Patients were included if they had an ICD-10 diagnosis code of I46 (cardiac arrest) and were treated with CPR at the scene. Exclusions were made for cases involving crime, suicide, trauma, or patients who died before EMS arrival or lacked recorded OHCA rhythm. Ultimately, data from 33,636 patients with OHCA were included in the analysis. Obesity status was determined using ICD-10 codes (E66) and descriptive diagnoses recorded by EMS personnel. Data from both the ICD-10 section and the descriptive diagnosis section of the medical records were used to categorize patients by sex and obesity status. The flowchart of patient is presented in Figure 1.
Data collection
Data were collected retrospectively from EMS records. The following variables were analyzed: sex, age, location of OHCA (non-public place vs public place, e.g., parks, streets, squares, sidewalks, libraries, schools, government buildings, public transportation facilities), initial rhythm, and presence of comorbidities such as HT, diabetes mellitus (DM), HF, history of cerebral stroke (CS), and ACS.
Variables
The primary outcome was the ROSC. Key exposures included obesity status, initial rhythm of OHCA (VF/pVT vs Asystole/PEA), location of OHCA (public place vs private place) and patient age. Comorbidities such as HT, DM, HF, CS, and ACS were also considered.
Bias
Efforts to minimize bias included using standardized ICD-10 codes for obesity and consistent methods of data collection across all EMS records. Potential sources of bias included the subjective assessment of obesity by EMS teams and the retrospective nature of the study.
Study size
The study included all available EMS records from the specified period, resulting in a final sample size of 33,636 OHCA patients.
Ethical considerations
The study was conducted according to the principles of the Declaration of Helsinki and was approved by the independent Bioethics Committee of Wroclaw Medical University, Poland (approval No. KB-895/2022). It also followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Statistical analyses
Data preprocessing and visualization were performed using Python 3.10.6 (https://www.python.org/downloads/release/python-3106/; packages: numpy 1.23.5, pandas 2.0.1, matplotlib 3.7.1, seaborn 0.12.2, and forestplot 0.3.1) in Visual Studio Code 1.80.0 (https://code.visualstudio.com/updates/v1_80). Statistical modeling was conducted with Statistica v. 13.3 (StatSoft Inc., Tulsa, USA) under a license provided by Wroclaw Medical University. The α value used for statistical inference was 0.05. Classical comparisons were performed with the independent samples t-test (by groups) or the χ2 test, depending on the compared data (continuous or categorical). Due to the large number of observations, the assumption of normal distribution was based on the central limit theorem (CLT), assuming that the variable (i.e., age) in both groups had a distribution that differed statistically insignificantly from the normal distribution. Homoscedasticity assumption was checked with the use of Levene’s test (Supplementary Table 1). If this assumption was not met, Cochran–Cox correction was applied to the t-test. In case of referring to variables of normal distribution, inherent moments of this distribution (mean and standard deviation (SD)) were chosen as descriptive statistics. In case of referring to variables of multinomial distribution, observed counts and frequencies were reported. In context of employing the χ2 test, the assumption that the estimated counts were not <5 in ≥20% of the cells of each contingency table was met.
Logistic regression (binomial distribution of the predicted variable, link function: logit, dummy coding) was used for statistical modelling to analyze the odds of ROSC. Since it was assumed that the variable in both groups had a distribution that was statistically insignificantly different from the normal distribution, the assumption of no outliers for logistic regression was not checked and it was considered to be met. Linearity assumption for the relationship between the continuous explanatory variables and the logit of the response variable was plotted and checked with use of Box–Tidwell test. Despite the violation of this assumption by the test results (p < 0.05), age was left untransformed in the models because the visible deviation from linearity was attributed to individuals of extreme age (i.e., >96 years).
Results
Sex and obesity-related differences in age, comorbidities and the incidence of ROSC
There was no difference in age, regardless of whether the group was subsequently stratified by sex only (Table 1) or by both sex and obesity status (Table 2). Obesity, DM, CS, HT, and HF were significantly more frequent among women. Conversely, ACS occurred more frequently among men (Table 1). Markedly, a nearly twofold higher incidence of the VF/pVT initial rhythm was observed among men (10.18% vs 5.47%, p < 0.001, Table 1). The difference in ROSC incidence between the 2 sexes was insignificant (p = 0.079, Table 1). Likewise, the frequencies of OHCA occurring in a public place were similar (p = 0.336, Table 1).
Upon subsequent stratification of the 2 sexes by obesity status, a markedly higher incidence of DM, HT and HF was observed, regardless of sex (Table 2). Although the obesity-related change in frequency of ACS and the VF/pVT initial rhythm was insignificant among women (p = 0.307 and p = 0.256, respectively), men showed higher incidence of ACS (p = 0.005) and lower incidence of the VF/pVT initial rhythm (p = 0.007) among the obese individuals, compared to non-obese (Table 2). There were no changes in the obesity-associated distribution of the location among the 2 sexes. Regardless of sex, ROSC occurred significantly less frequently among obese individuals (30.35% vs 35.35% among women and 32.19% vs 36.25% among men).
Exploring the modulation of the odds of ROSC by obesity – insights from univariate and multi-factor models
According to the univariate model (Table 3), obesity decreased the odds of ROSC by 25.47% among women (p = 0.034) and 19.76% (p = 0.035) among men. Upon adding other features to the model, obesity became insignificant (Table 3). However, it was on the brink of statistical significance (p = 0.051) among women, according to the model adjusted by 3 key factors modulating the odds of ROSC: initial rhythm, location, and age. According to models with all factors (Table 3), the individuals with the VF/pVT initial rhythm were 4.204-fold more likely (vs Asystole/PEA) to develop ROSC among women, but only 3.655-fold more likely among men. If OHCA happened in a public place, both sexes showed similar, over twofold increase in odds of ROSC (2.204 among women, 2.130 among men). The association of age on these odds was similar among the 2 sexes, decreasing the odds for ROSC (by 1.21% and 1.52% in women and men, respectively, per 1-year increase in age). Moreover, unlike men (p = 0.832), women showed a 10.01% decrease in the odds for ROSC upon the presence of hypertension (p = 0.044).
After stratification by sex and obesity (Table 4), several factors appeared to influence the odds for ROSC differently. Although the public place location significantly increased the odds for ROSC among both sexes, women showed to have significantly lower location-associated OR if they were obese (2.126 vs 4.264 in woman with obesity and without, respectively). Moreover, exclusively among non-obese women, hypertension decreased the odds of ROSC by 11.11% (p = 0.032).
Discussion
The study aimed to assess the association of obesity with the incidence of ROSC among OHCA patients, specifically in context of between-sex differences. Regardless of sex, ROSC occurred significantly less frequently among obese individuals, as observed in several studies.4, 12, 30 Despite corroborating evidence found in scientific literature, the most solid studies indicate that obesity is a factor which increases the risk of mortality in patients with OHCA since it decreases the probability of ROSC, increasing the deterioration of the vascular system or making CPR difficult.3, 4, 12, 30, 35, 36 In this study, the term “obesity” refers to patients described as obese by EMS teams based on available information, which may include visual assessment or medical records. This approach, while necessary in the urgent context of OHCA, may introduce a degree of subjectivity that could affect the accuracy of obesity categorization. It is important to note that measuring weight and height in these urgent and vulnerable situations is not always feasible, and these parameters are often determined upon taking a glance at the patient. This limitation should be considered when interpreting the results of our study. Our univariate analysis showed a significant association between obesity and decreased odds of ROSC, but the multivariate analysis indicated that this association was not statistically significant. It is important to note that this loss of significance in multivariate settings does not necessarily mean that obesity does not modulate the odds of ROSC in real-life settings. The more rational conclusion would be that other factors, such as initial rhythm and location of OHCA, may play a more critical role in influencing ROSC outcomes,37, 38 compared to obesity status.
This study, along with research by Fehler et al.,5 Czapla et al.,3, 4 Tanaka et al.,17 and Haskins et al.,39 not only analyzed but also observed that patients presenting with VF/pVT had a higher likelihood of ROSC. When we consider the differences between sex, we have seen an almost twofold higher incidence of the initial VF/pVT rhythm among men, which has been reported in other studies.18, 23, 24 Although other investigators have reported that in their population samples, women were generally older than men, there was no difference in age between both sexes in our data. The low survival rate among women is driven by higher prevalence of chronic diseases (DM, HT, CS, CVD) and a greater occurrence of OHCA at home or without witnesses.18, 22 Moreover, the presence of obesity among women statistically significantly decreased the effectiveness of CPR among women with obesity experiencing OHCA in a public place. Not only are women less likely to experience OHCA in a public place, but they are also negatively affected by obesity in terms of being subject to effective CPR in public places.21, 23, 24, 25 The most significant predictors of ROSC in our study were the initial VF/pVT rhythm and the occurrence of OHCA in a public place. Women with an initial VF/pVT rhythm had a 4.204 times greater chance of achieving ROSC, compared to a 3.655-fold difference found among men. Additionally, OHCA in a public place increased the odds of ROSC more than twofold for both sexes. These findings highlight the paramount importance of initial rhythm and the context of the arrest location over the isolated effect of obesity.
In our results, we have seen how an increase of 1 year in the age of the patients similarly decreases the probabilities of ROSC between both sexes, just as we observed in our previous study5 and the rest of the studies of the scientific literature,2, 4, 17, 40 with similar values among all the results, but with the lack of taking gender differences into account in case of studies performed by other investigators. Other studies have reported that although the association of age affects both sexes equally, in the phase after cardiac arrest, older women showed a higher mortality rate compared to men.40 However, when women of premenopausal age were compared with men of the same age, the former had higher levels of survival.27, 40, 41, 42 Awad et al. only described this difference in the group of women with initial non-shockable heart rhythm.40 We can observe the cumulative effect of chronic diseases in our multivariate analysis since women with hypertension showed a 10% decrease in the odds of ROSC, which increases the number of deaths in women, in contrast to the data obtained in our previous study, where no difference was made between sexes, and hypertension only showed a decrease of 3.4%.5 Stratification by age and sex also showed an 11% decrease in the odds of ROSC among non-obese women, with a smaller reduction seen in all non-obese patients in our previous study.5 Considering solely the obesity factor, we once again observed that the female sex is the most affected since this pathology decreased the probabilities of ROSC by 25.47% vs the reduction of 19.76% among men. However, in the multivariate analysis taking all factors into account, women with initial VF/pVT rhythm were more likely to develop ROSC than men with the same type of initial rhythm, which opposes the previous results.4, 18, 25, 39 The mentioned studies did not consider the association of obesity on the ROSC, highlighting a need for further research in this aspect. Our results indicate that while obesity has a significant impact in univariate analysis, its effect is mitigated when other critical factors are considered in a multivariate context. This aligns with recent studies that question the so-called “obesity paradox” in cardiac arrest outcomes. Therefore, our findings contribute to a growing body of evidence suggesting that the role of obesity in ROSC is complex and influenced by multiple interacting factors.
The reported results, including those found in the scientific literature,18, 22, 23, 24, 25, 43 show differences in the prevalence of OHCA between women and men, as well as the associated pathologies or the diagnosis and treatment they receive. Most studies indicate that women are more likely to experience OHCA with associated pathologies.15, 18, 22, 25 Additionally, they show lower survival rates or worse associated outcomes.18, 22, 23, 25 Our findings confirm the differences observed between both sexes. Since obesity, in particular, makes CPR more difficult in the case of women, new approaches must be adopted in the treatment of OHCA. The fact of finding some contradictory results, such as the higher frequency of initial VF/pVT rhythm among women, highlights the need to investigate sex-associated variability and adopt measures that improve survival rates among the female sex; when women receive the correct measures, they show a better recovery than men.23, 27
Implications for practice
Given these findings, it is essential for clinical practice to prioritize factors which have a more direct and substantial impact on ROSC outcomes, such as ensuring rapid defibrillation and effective CPR, especially in public settings. While addressing obesity remains important for overall cardiovascular health, it may not be the most critical factor in the acute setting of OHCA. Our results are in line with the available scientific literature that describes a higher prevalence of CVD among women and worse survival outcomes related to OHCA, derived from a greater odds of occurring.22, 25, 26, 27, 44 These events occur when the women are alone at home without the presence of witnesses or have a lower frequency of shockable rhythms.4, 17, 27 Additionally, it has been observed that women receive fewer invasive treatments once they are admitted to the hospital after experiencing OHCA, which leads to worse health outcomes. Other studies have indicated that health illiteracy, older age of women or low socioeconomic status of women are correlated with an underestimation of CVD risk.27 These facts, together with the greater prevalence of chronic diseases in women, such as obesity, negatively influence treatment and success rates for ROSC among women with OHCA. It is necessary to include a sex-related approach in the care of women with OHCA, and in general with any disease, since we see worse health outcomes associated with the female sex. Furthermore, improving the accuracy of obesity recognition and its documentation in medical records is crucial. This could help in better understanding the impact of obesity on OHCA outcomes and in developing targeted interventions to improve survival rates. In this context, prospective studies should be conducted to assess the impact of obesity on OHCA outcomes. This approach would provide a more comprehensive understanding of the role of obesity in OHCA and help in formulating effective strategies to enhance patient outcomes.
Limitations
This study has several important limitations. The assessment of obesity by EMS personnel, based on available information such as visual evaluation, medical records, ICD-10 codes (E66), and descriptive diagnoses recorded, may introduce some inaccuracies. We do not have detailed information on how the diagnosis of obesity (E66) was determined, whether through direct measurements or visual assessment. It is likely that only patients who appeared overtly obese were categorized as such. This limitation should be considered when interpreting the findings, as it may impact the accuracy of the obesity categorization. This method of assessment may lead to an underestimation of obesity prevalence compared to studies using precise BMI measurements. Additionally, due to the retrospective nature of this study and the emergency context in which EMS personnel operate, it was not possible to obtain precise measurements of BMI, body composition or other detailed anthropometric data. The retrospective nature of this study and the characteristics of the database used introduce additional limitations. One concern is the uncertainty surrounding the data associated with comorbidities, as the EMS staff might not have interacted with family witnesses or had access to the patient’s medical history. The emergency medical records lacked specific information on whether bystanders-initiated CPR before the arrival of the medical team, as well as the duration of such CPR, making it impossible to incorporate these factors into the analysis. Additionally, our dataset did not include detailed time-related data such as EMS response times, activation of the emergency system and bystander use of automated external defibrillators (AEDs). Our dataset also lacked specific clinical parameters like end-tidal carbon dioxide (ETCO2) values, which are increasingly recognized as important prognostic markers in cardiac arrest. Moreover, there was limited information on airway management, including successful intubation rates and the use of alternative airway devices in cases of failed intubation attempts, particularly among obese patients. The anonymity of medical records precluded the examination of long-term survival. However, it is essential to note that a notable strength of the study lies in its extensive sample size, encompassing the entire Polish population.
Conclusions
Our study demonstrated that obesity was not an independent predictor of ROSC in OHCA patients. Different predictors of ROSC were identified for men and women. Major findings from this study indicate that initial VF/pVT rhythm and occurrence of OHCA in a public place significantly increase the likelihood of achieving ROSC. Women with an initial VF/pVT rhythm had a 4.204 times greater chance of ROSC compared to 3.655 times increase in men. Among both sexes, increasing age was associated with decreased odds of ROSC. These factors had a more significant impact on ROSC outcomes than obesity.
Further research is necessary to better understand the underlying mechanisms driving these differences and to develop targeted interventions that can enhance the effectiveness of resuscitation efforts for all OHCA patients.
Supplementary data
The Supplementary materials are available at https://doi.org/10.5281/zenodo.13754402. The package includes the following files:
Supplementary Table 1. Detailed report on models related to location and initial rhythm, including ORs and 95% CIs for cardiac arrest outcomes.
Supplementary Table 2. Further analysis of initial rhythm and location, adjusted by sex, age and other factors affecting cardiac arrest outcomes.
Supplementary Table 3. Assessment of multicollinearity between variables used in logistic regression models, based on the variance inflation factor (VIF).
Supplementary Table 4. Results of a 3-way logistic regression model showing the combined effects of sex, location and initial rhythm on the odds of ROSC.
Supplementary Table 5. A logistic regression model demonstrating how location and age modulate ROSC odds, with and without interaction with initial rhythm.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.