Abstract
Background. The focus on health-related quality of life (HRQOL) in medical research is becoming more and more intensive, with attention being paid to the patient’s subjective feelings and assessment of one’s health status. Smell disorders can significantly impact human life. The Questionnaire of Olfactory Disorders (QOD) is a self-monitoring questionnaire that provides subjective information about olfactory disorders.
Objectives. This study aimed to check the reliability and validation of the Polish version of QOD (QOD-PL) for use in patients with olfactory impairment in Poland.
Materials and methods. A total of 158 patients (76 females, mean age (Mage) 45.97 ±16.37 years), suffering from chronic rhinosinusitis (CRS), whose olfactory function was measured using the Sniffin’ Sticks test (SST), were studied. All patients completed 3 validated questionnaires: Importance of Olfaction (IO), Sino-Nasal Outcome Test–22 (SNOT-22) and QOD-PL.
Results. Internal consistency and test-retest reliability of the entire QOD-PL scale were good (Cronbach’s α = 0.88). The convergent validity of the QOD-PL and its subscales correlated with IO and SNOT-22. The life quality statements in the QOD-PL (QOD-PL-LQ) score, its negative statements, and the mean score for VAS scales were significantly and positively correlated with all symptoms measured with SNOT-22 and none of the IO scales.
Conclusions. The QOD-PL is a reliable, valid and important tool for assessing HRQOL in patients with olfactory disorders. However, it is important to note that not all of its subscales can be considered and interpreted separately.
Key words: quality of life, questionnaire, olfaction disorders, smell, patient-reported outcome measures
Background
The focus on the health-related quality of life (HRQOL) in medical research is increasing, with attention being paid to the patient’s subjective feelings and assessment of one’s health status. The patient’s self-assessment plays an essential role in the treatment process and the effectiveness of the undertaken therapy.1, 2 Smell disorders can significantly impact human life,3, 4 yet olfactory dysfunction is consistently undervalued by patients and disregarded by physicians.5, 6 When the sense of smell is impaired or completely absent, food intake is disrupted, and the critical alarm system toward environmental hazards such as gas leakages or spoiled foods becomes dysfunctional. Furthermore, human social communication becomes impaired when the sense of smell is not functioning.7 People affected by smell loss (anosmics) are more likely to suffer from psychological problems such as depression. It is estimated that this affects 1 in 4 patients with olfactory disorders.8, 9
The growing interest in olfaction-related quality of life (QoL) resulted in a dedicated measurement tool – the Questionnaire of Olfactory Disorders (QOD).3 It is a self-monitoring questionnaire that provides subjective information about olfactory disorders. Furthermore, QOD has been shown to have greater specificity in assessing olfaction-related QoL as compared to other instruments, such as the 36-item Short Form Health Survey (SF-36).10 Monitoring the consequences of olfactory disorders is of particular importance now, in the post-COVID era, when many people struggle with post-infection anosmia. Furthermore, the COVID-19 pandemic has drawn global attention to the large-scale problem of sudden olfactory loss11, 12 and the associated reduction in QoL.13 Therefore, there is an urgent need to monitor changes in the sense of smell and the severity of these changes in daily life by means of a questionnaire since the loss of smell is a non-specific symptom, and the use of objective tests is problematic.
Objectives
Since QOD is not available in Polish and has no normative data for the Polish population, the present study aimed to check the reliability and validation of the Polish version of QOD (QOD-PL; Supplementary file available at https://doi.org/10.5281/zenodo.8263258) for use in patients with olfactory impairment in Poland.
Materials and methods
Participants
A total of 158 people participated in the study, of which 115 were in the study group and were patients with chronic rhinosinusitis (CRS), while the remaining 43 healthy subjects (without olfactory disorders, sinus disease or other chronic diseases) were in the control group. The study participants were recruited at the Department of Otolaryngology, Head and Neck Surgery of the University Hospital in Wrocław, Poland. The diagnosis was established based on the medical history and a clinical examination, including nasal endoscopy, and complemented with diagnostic imaging – computed tomography (CT) of the sinuses. Patients with malignancy, cystic fibrosis, severe head trauma, or significant neurological or psychiatric disorders were excluded (Figure 1). Based on the subject’s olfactory performance quantified with the Sniffin’ Sticks battery (SST test),14 we categorized them as functionally anosmic (<16 points) or hyposmic (<30.75 points). The parosmia assessment was based on a QOD-PL questionnaire only.
Procedure
Patients included in the study completed 3 questionnaires: 1) QOD-PL, 2) Importance of Olfaction (IO) test15 and 3) Sino-Nasal Outcome Test – 22 (SNOT-22).16 The patients completed the QOD-PL twice (test and re-test) at intervals of a minimum of 14 days, prior to surgery or after significant modifications in treatment. The original English version of the QOD questionnaire was translated and adapted to Polish according to internationally accepted guidelines.17, 18 Two native speakers of Polish who were also fluent in English and familiar with Polish culture translated the original English version of the QOD questionnaire into Polish. A 3rd independent expert compared the 2 translated versions, reaching a consensus. A sequentially coherent version was re-translated into English by 2 native speakers of English who were also experts in Polish and familiar with the country’s culture. The translated questionnaire was then compared with the English original. The process was repeated until a consensus was reached, and a final version of the Polish QOD-PL questionnaire was created. Similar to the original QOD questionnaire, the Polish adaptation (QOD-PL) consists of 2 parts. The 1st part contains 29 statements divided into 3 subscales: life quality statements (LQ, QOD-PL-LQ), “socially desirable” responses (Sincerity statements, QOD-PL-SS) and parosmia assessment (Parosmia statements, QOD-PL-Parosmia), as shown in Table 1. The 2nd part of the test consists of 5 visual analogue scales (QOD-PL-VAS; Supplementary file available at https://doi.org/10.5281/zenodo.8263258). The QOD-PL-LQ expresses the patient’s complaints related to olfactory disorders. They consist of 19 statements – 17 “negative” (so-called negative statements (QOD-PL-NS) and 2 “positive statements” (QOD-PL-PS). For each statement, the respondent gives one answer by marking respectively: “agree”, “partially agree”, “partially disagree”, or “disagree”. Each response is assigned 3, 2, 1, or 0 points, respectively, for NS and reverse scoring for PS. The total score for the Quality of Life (LQrv) assessment can reach 57 points. The LQrv converts to a QoL score. Higher scores indicate a more significant deterioration in the QoL. Statements from the SS subscale indicate whether patients provide the expected information and how reliable their indicated responses are in relation to this. Low scores indicate a tendency to give socially desirable answers. Points for the parosmia assessment are assigned analogously to the QoL-NS. High scores indicate parosmia. The part of the VAS of the questionnaire assesses difficulties with smell using 5 VAS. These relate to how annoying the smell difficulties are (1), how often patients are aware of how annoying the smell difficulties are (1), how often the patients are aware of them (2), to what extent they are affected at their work (3) and on their leisure time (4) and private life (5). The summary and scoring key for QOD-PL are shown in Table 1.
The IO questionnaire by Croy et al. aims to determine the differences in the subjective perception of the sense of smell among patients.15 The form consists of 20 statements to which one response must be indicated on a 4-point scale from “completely agree” to “completely disagree”. Accordingly, 6 statements each form 3 subscales: Association (IO-Ass), Application (IO-App) and Consequence (IO-Con). The other 2 belong to the Aggravation subscale. The questionnaire’s authors demonstrated its usefulness for normosmia, hyposmia and anosmia.
Sino-Nasal Outcome Test – 22 (SNOT-22),16 the commonly used questionnaire for the assessment of QoL in rhinosinusitis, was obtained from the author with permission to use it.19 The first version of this questionnaire was published in 2002 as SNOT-20 by Piccirillo et al.20 It was then modified in 2009 by Hopkins et al. and named SNOT-22.16 This tool is used to assess the severity of symptoms and complaints in CRS and their impact on the patient’s HRQOL. The SNOT-22 covers a wide range of health problems, including physical problems, functional limitations and emotional consequences resulting from persistent complaints. The questionnaire consists of 22 statements to which responses are assigned on a 5-point scale: 0 – no problem, 1 – a very minor problem, 2 – a minor problem, 3 – a moderate problem, 4 – a severe problem, and 5 – worst possible problem. The maximum possible score is 110 points. The higher the sum of the scores obtained, the more significant the complaints of CRS are and the greater the negative impact on the patient’s QoL. In the 2nd part of the questionnaire, the respondent is asked to mark 5 of the listed complaints that have the greatest impact on their health. DeConde et al. distinguished 5 domains in the SNOT-22 questionnaire. Three of them are specific to sinus complaints (i.e., rhinological symptoms, extra-nasal symptoms and ear-facial symptoms) and 2 general domains related to HRQOL – psychological and sleep disturbance domains.21 When comparing the questionnaires with each other and assuming that the validated questionnaire is working properly, positive correlations are expected between QOD-PL and SNOT-22; it can be assumed that the relationship between QOD-PL and IO will be inversely proportional or neutral.
Statistical analyses
Data were analyzed using IBM SPSS v. 26 software (IBM Corp., Armonk, USA) with the level of significance set to α = 0.01 to correct for multiple comparisons and reduce the risk of false positive results (type I errors). The internal consistency of the QOD and its subscales was assessed using Cronbach’s α coefficient, and the values of 0.70–0.9522 were considered satisfactory. Data distribution was confirmed to differ from normality, as indicated by the significant result of the Kolmogorov–Smirnov test (p < 0.01). Therefore, we used non-parametric tests. Intergroup differences in age were assessed utilizing the Kruskal–Wallis test. The test-retest reliability examined the absolute agreement between the measurements with the two-way mixed intraclass correlation coefficient (ICC). The convergent validity of the QOD-PL was assessed by examining the correlation between its scores with the SNOT-22 and IO questionnaire scores and the SST test for olfactory dysfunction, using the Spearman’s rho (rs) partial correlation coefficient (controlling for rhinological symptoms measured with SNOT-22). Finally, the discriminative validity of the QOD-PL was evaluated by comparing its scores between subgroups of patients with different olfactory functions (anosmics, hyposmics and normosmics) using the Kruskal–Wallis test as well as between patients with CRS compared to healthy controls utilizing the Mann–Whitney U test.
Ethical considerations
The ethics review board of Wroclaw Medical University approved the study design and consent approach (approval No. KB – 259/2017). The study was conducted in accordance with the Declaration of Helsinki on Biomedical Studies Involving Human Subjects. Informed written consent was obtained from all participants, who were volunteers and were aware of the study’s aim, design and clinical implications.
Results
Participants
A total of 158 subjects aged between 19 and 87 years participated in this study (median age (Mage) = 45.97 ±16.37 years, 76 women), of whom 115 subjects were patients with CRS (without/with nasal polyps; Mage = 49.4 ±15.4 years, 51 women). The control group was 43 healthy subjects (Mage = 36.7 ±15.4 years, 25 women).
Sex was distributed independently from olfactory performance (χ2 = 4.1. p = 0.13). There was a significant effect of the group on age (H(2) = 37.5, p < 0.001), suggesting that the anosmic and hyposmic groups were significantly older than the normosmic group (p < 0.001) but not different from each other (p = 0.618). All 43 healthy subjects’ SST scores fell into the range of normosmia (≥30.75 points).23 Descriptive statistics for the 3 groups are summarized in Table 2.
The reliability of the entire QOD-PL scale was good (Cronbach’s α = 0.88). Reliability of the QOD-PL-NS was excellent, as reflected by Cronbach’s α = 0.94, yet the reliability of QOD-PL-PS was poor with Cronbach’s α = 0.50 (for QOD-LQ jointly Cronbach’s α = 0.88 suggesting overall good reliability), reliability of QOD-PL-SS was poor with Cronbach’s α = 0.53, and QOD-PL-Parosmia Cronbach’s α = 0.70 suggested satisfactory reliability, while VAS scales presented good reliability with Cronbach’s α = 0.86. The ICCs and the results of the paired samples t-tests are summarized in Table 3.
Correlation between QOD-PL
and IO and SNOT-22
The convergent validity of the QOD-PL and its subscales were correlated with IO and SNOT-22. The QOD-PL-LQ score, its negative statements and the mean score for VAS scales were significantly and positively correlated with all symptoms measures with SNOT-22 and none of the IO scales (Table 4). QOD-PL-PS and QOD-PL-SS were not related to IO or SNOT-22. Statistical coefficients and the level of significance are summarized in Table 4.
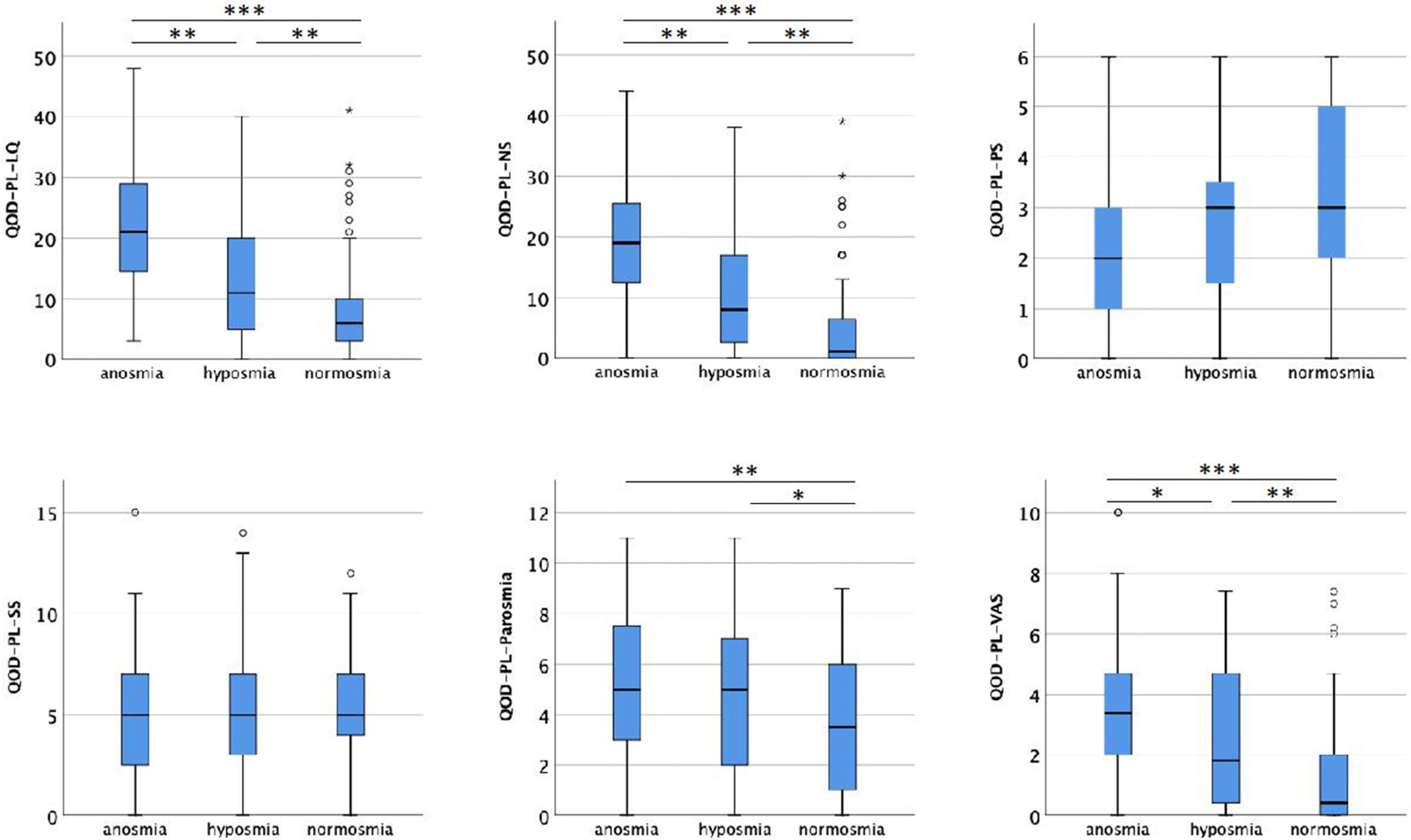
The discriminant validity was assessed by examining the intergroup differences in QOD-The PL scores for subjects with anosmia, hyposmia and normosmia. We found significant intergroup differences for the total QOD-LQ score and its negative statements (QOD-PL-NS) and VAS scales. The questionnaire also differentiated subjects with normosmia from both groups exhibiting olfactory deficits in terms of parosmia symptoms. Positive and sincerity statements did not yield any differences between subjects with anosmia, hyposmia and normosmia. However, healthy controls scored lower than CRS patients in the QOD-PL-NS (mean rank (Mrank) = 94.5 compared to M rank = 39.3, U = 744, p < 0.001, respectively), QOD-PL-LQ (Mrank = 94 compared to Mrank = 40.7, U = 805.5, p < 0.001), QOD-PL-Parosmia (Mrank = 87.9 compared to Mrank = 57.1, U = 1510, p < 0.001), and QOD-PL-VAS (Mrank = 97.2 compared to Mrank = 48.3, U = 1130.5, p < 0.001); and healthy controls scored higher than CRS patients in QOD-PL-SS (Mrank = 87.9 compared to Mrank = 76.4, U = 2834, p < 0.001), corroborating the comparison between anosmic, hyposmic and normosmic groups (Figure 2).
Subjects with CRS diagnosis
There were no significant sex-related differences in any of the QOD-PL subscales (all p > 0.13). Age was positively related to QOD-PL-NS (rs = 0.22, p = 0.006) and QOD-PL-Parosmia (rs = 0.25, p = 0.001), suggesting that olfaction-related complaints and parosmia increase with age. On the contrary, the QOD-PL-PS score was negatively related to age (rs = −0.16, p = 0.049), indicating worse coping with olfactory loss in older subjects. Examination of the relationships between QOD-PL scores and olfactory performance while controlling for rhinological symptoms revealed a significant negative relationship between QOD-LQ scores (driven by the QOD-PL-NS subscale), indicating that stronger complaints were recorded with the questionnaire (i.e., higher QOD-PL scores), the poorer olfactory performance was measured with the SST test. The QOD-PL-VAS was negatively associated with odor identification, suggesting that lower scores on the QOD-PL-VAS related to the lower ability to name odorants. No relationship was found between the QOD-PL-PS, QOD-PL-SS and QOD-PL-Parosmia and olfactory performance. Spearman’s rho correlation coefficients are presented in Table 5.
Discussion
The results of our study showed that the QOD-PL had good reliability and accuracy, making this questionnaire in our translation a reliable and valid tool for otolaryngological assessments of the QoL. Moreover, a poorer smell-related QoL (QOD-PL) correlated with scores on the more objective SST test. In the next steps of the tool’s development, QOD-PL should be included in clinical trials to see if an improvement in the QoL (as measured with QOD-PL) follows various interventions, including surgical. However, this component was not part of this study.
We observed relatively lower psychometrical values for the QOD-PL-PS. The questionnaire authors obtained similar values for Cronbach’s α coefficients for the QOD-PS components at 0.054,3 while a slightly higher value of Cronbach’s α for this component (0.69) was obtained by the authors of the questionnaire’s adaptation into Greek.10 Following other research groups, it is possible to use only the negative scale (QOD-NS),24, 25 with the partial omission of the positive scale, and this should not have significant consequences for the reliability of the results, but we suggest empirically testing it in Poland.
A comparison of QOD-PL and SNOT-22 scores in the same group of patients showed statistically significant correlations between smell-related QoL and all domains of the SNOT-22 questionnaire, i.e., rhinological symptoms, extra-nasal symptoms, ear/facial symptoms, psychological dysfunction, and sleep dysfunction. In conclusion, as CRS disease severity-related QoL deteriorates, olfactory-related QoL declines. Therefore, the expected relationship between QOD-PL and SNOT-22 proves the external validity of QOD-PL in the Polish population.
A comparison of QOD-PL and IO scores showed no significant correlation. This may be explained by the fact that functional anosmic patients, compared to normosmic subjects, both healthy and CRS patients, place statistically significantly less importance on using the sense of smell during daily activities.26, 27 This simultaneously indicates a successful adaptation of these patients to the disorders of the sense of smell. At the same time, normosmic patients tend to exaggerate the importance of the sense of smell. This may be due to the sudden, temporary deterioration of the ability to smell due to the severity of the CRS lesions, which is associated with a lack of adaptation to the changes and, consequently, a lack of acceptance of the loss of smell.26 Hence, the IO questionnaire alone should not be used to monitor olfactory impairment.
Limitations
The study included patients with the same cause of olfactory disorders, and it would be worthwhile in the future to test the questionnaire’s performance for different reasons of disorders.
Conclusions
The QOD-PL is a reliable, valid and important tool for assessing HRQOL in patients with olfactory disorders. However, when the subgroups of this questionnaire are considered separately, the negative statement domain of QOD-PL can be analyzed independently and the positive statements part of the QOD-PL should not be considered individually for any interpretation. Nevertheless, to the authors’ knowledge, it is the only tool currently available in the Polish population to assess the QoL and to measure problems related to olfactory impairment.