Abstract
Background. Amputation followed by index finger pollicization is the gold-standard treatment for type III B thumb hypoplasia. However, despite its high success rate, some parents decline this procedure because it results in a four-finger hand.
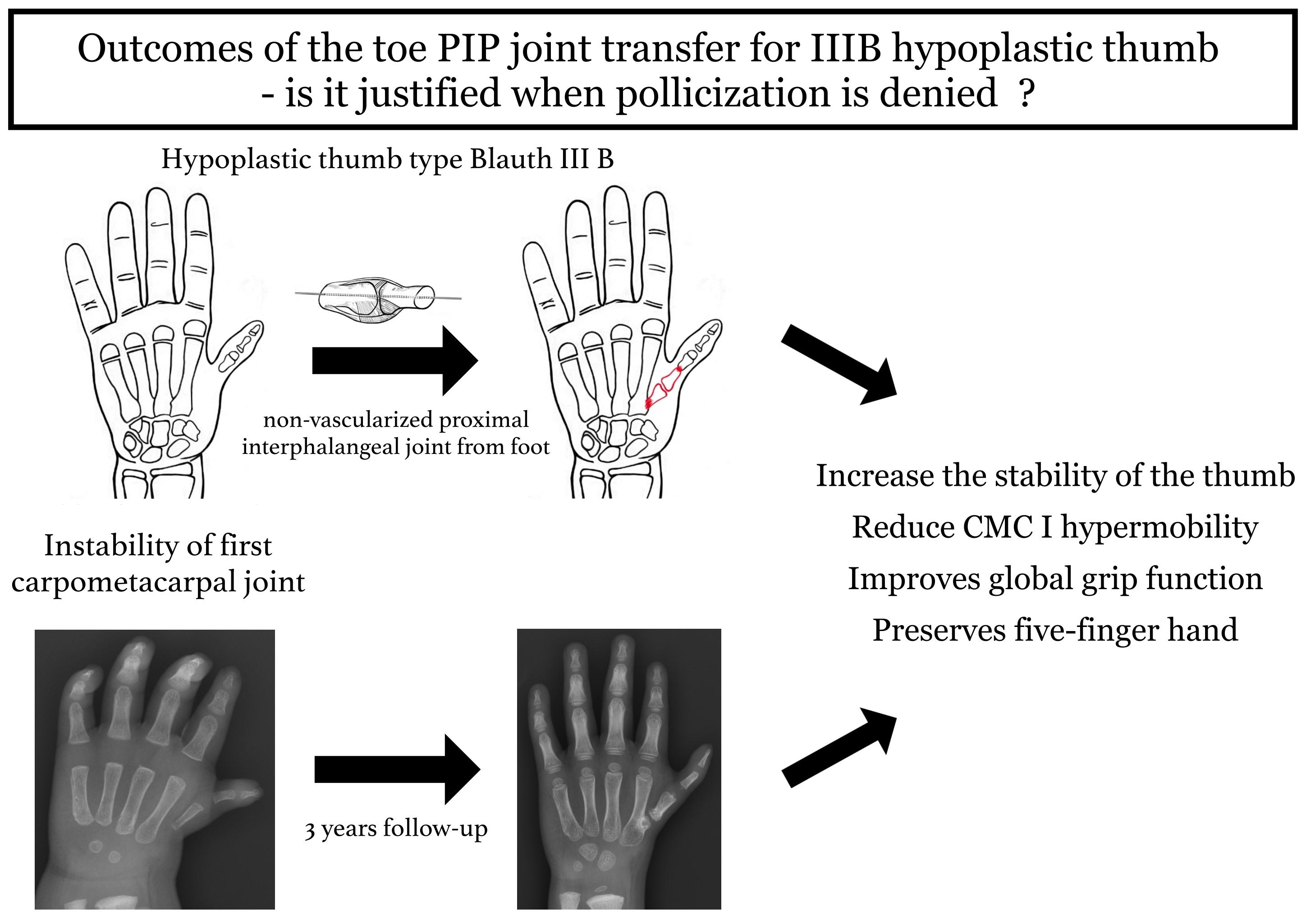
Objectives. To evaluate the outcomes of reconstructive surgery in eight patients with type III B thumb hypoplasia, stabilized using a non-vascularized proximal interphalangeal (PIP) joint harvested from the foot when parental consent for pollicization was not granted.
Materials and methods. The study cohort comprised 8 postoperative patients (mean follow-up: 7 years) who underwent reconstructive stabilization of a hypoplastic thumb using a PIP joint from the foot. Hand function was evaluated by measuring range of motion (ROM), thumb stability and length, grip strength, and performance on a manual manipulation test. Donor-site morbidity was assessed via foot examination following PIP joint harvest. Functional outcomes were further analyzed using specialized patient-reported questionnaires.
Results. Most patients achieved good thumb stability and a functional passive range of motion. Reconstructed thumbs averaged approx. 75% of the length of a normal thumb, and grip strength measured about 50% of that in the contralateral hand. Donor-site assessment revealed toe shortening in the majority of cases but no deficits in ambulation or weight-bearing. The overall complication rate was 25%, and most patients and their parents reported satisfaction with the treatment.
Conclusions. Thumb reconstruction with a non-vascularized PIP joint yields enhanced stability and reduced hypermobility, with outcomes comparable to those reported for similar techniques. This approach represents a viable alternative for patients whose parents decline pollicization.
Key words: proximal interphalangeal joint, Blauth IIIB, PIP joint transfer, thumb stabilization, thumb hypoplasia
Background
Congenital disabilities affect approx. 1% of newborns, and upper limb anomalies account for about 10% of these cases. Thumb hypoplasia or aplasia, a form of radial longitudinal deficiency, represents only 11% of all hand anomalies. This condition can occur as an isolated defect or in association with syndromes such as Holt–Oram, Rubinstein–Taybi, Apert, VACTERL association (vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities), Fanconi anemia, or congenital radial deficiency.1, 2, 3
The modified Blauth classification system, which relies on clinical assessment and radiographic imaging, is used to determine the severity of thumb hypoplasia and guide the choice of surgical intervention.4, 5 Thumb hypoplasia significantly compromises hand grip function, thereby impacting both the physical and mental development of affected children.6 Surgical intervention plays a key role in reducing disability, supporting development, and minimizing everyday functional limitations. Early treatment is critical to avoid maladaptive grip patterns, which can hinder rehabilitation and proper grasp development once embedded in the brain’s cortical representation.6, 7, 8
The choice of surgical procedure depends on the severity of the thumb defect, and cosmetic and ethical factors are also considered, which increasingly influence parents’ decision-making.5, 9, 10, 11 In cases of type III B thumb hypoplasia, as classified by the modified Blauth system, the condition is marked by thumb shortening and narrowing, flattening of the thumb web space, and underdeveloped thenar muscles. Additional characteristics include underdevelopment of the flexor pollicis longus (FPL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and abductor pollicis longus (APL) tendons, as well as the proximal 2/3 of the first metacarpal, coupled with instability of the metacarpophalangeal (MP) and carpometacarpal (CMC) joints. The preferred treatment for this defect is thumb amputation followed by pollicization of the index finger, which delivers good functional outcomes and high patient satisfaction rates.2, 12, 13, 14, 15
Although effective, thumb amputation is often declined by parents because it results in a 4-fingered hand. The literature provides limited data on reconstructive methods to stabilize hypoplastic thumbs, where hypermobility and instability are major causes of dysfunction.9, 10, 11, 16, 17, 18, 19, 20, 21, 22, 23
Objectives
This study aimed to evaluate the outcomes of reconstructive surgery in 8 patients who underwent thumb stabilization procedures using a non-vascularized PIP joint harvested from the foot. These procedures were performed only in cases where parents declined pollicization.24
Materials and methods
Study design
This is a retrospective study evaluating the objective and subjective outcomes of surgical treatment of patients from the hand surgery department, with a minimum follow-up of 1 year. The data were summarized and interpreted, and appropriate conclusions were drawn, comparing the results with similar alternative treatment techniques in the literature.
As part of the basic statistical evaluation, the median value of the studied variables was presented, and, additionally, a correlation analysis was performed using Spearman’s correlation coefficient. The confidence interval at which a result was considered statistically significant was adopted for p < 0.05.
Ethical approval was waived by the institute’s Bioethics Committee, which determined that this study did not constitute a medical experiment requiring formal review. The research was conducted in accordance with the Declaration of Helsinki (2013 revision).
Participants
Between 2000 and 2022, our hand surgery department treated 25 patients with type III B thumb hypoplasia whose parents declined gold-standard pollicization – due to the resulting 4-fingered hand – and instead opted for alternative reconstructive techniques. For this reason, we proposed and performed an alternative reconstructive surgery by stabilizing the hypoplastic thumb using a non-vascularized PIP joint from the foot. An additional inclusion criterion required that the affected thumb have no history of prior surgical intervention. The surgical technique and related procedural details have been described comprehensively in an earlier publication (Figure 1).24
Eight patients participated in the study, including 4 girls (50%) and 4 boys (50%), aged 3–15 years, with an average age of 8 years and 6 months. The defect was unilateral in 7 cases and an isolated thumb defect in 5 cases. Three cases involved a complex upper extremity defect, such as congenital radial deficiency. One patient had additional diagnoses of congenital hearing loss, hydrocephalus, and thumb aplasia in the contralateral hand. The children underwent between 1 and 4 surgeries (median: 1.5), with thumb stabilization using PIP joint graft often being the 1st procedure performed. Additional procedures included wrist centralization and ulnar bone lengthening. The age at the time of surgery ranged from 1 year to 3.5 years, with the median age of 1 year. Five right hands and 3 left hands underwent surgical procedures. The donor PIP joint was harvested from the right foot 7 times and from the left foot once. In 75% (6/8) of the cases, the grafts were obtained from the same side as the operated hand. The 3rd toe was most frequently used as the donor site, accounting for 63% of the cases, while the 4th and 2nd toes were used as the donor sites in 25% (2) and 12% (1) of the cases, respectively. One patient (No. 7) underwent a Huber opposition transfer 1 year after receiving the non-vascularized PIP joint graft from the toe to the hypoplastic thumb.25
The follow-up period ranged from 1 to 13 years, with a median of 6.5 years. Detailed patient data are provided in Table 1.
Methods
The study on children and adolescents strictly adhered to ethical guidelines and the principles outlined in the Declaration of Helsinki. Before the commencement of the study, the entire process was thoroughly explained and presented to both the parents and the children. Participation in the study was entirely voluntary, and verbal consent was obtained from all the participants and their legal guardians, most often one of the parents. Ethical approval was waived by the Bioethics Committee of Poznan University of Medical Sciences, which issued a written waiver confirming that formal ethics review was not required for this non-experimental study
The first author examined all the patients under the supervision of the specialist. As part of the functional assessment, the passive range of motion in all joints of the hypoplastic thumb was measured using a goniometer and the point of maximum opposition. The stability of the transferred joint was evaluated with the dorsal shift test. It was performed by creating longitudinal traction to the thumb and then applying a palmar and dorsal pressure over the base of the 1st metacarpal to provoke subluxation of the joint.26, 27
Sensation on the fingertip was assessed considering sensory discrimination using a standard 2-point discriminator.
The relative length of the hypoplastic thumb compared to the index finger was measured using the method developed by Goldfarb et al.28 The norm refers to an adducted thumb, where the fingertip reaches 70% of the proximal phalanx length (AD/AB length ratio) and 32% of the index finger length (AD/AC length ratio).
The strength of the global and precise 2-point grip was assessed using equipment from Biometrics Ltd. E-LINK, Newport, UK; we used a Hand Accessory Kit (H400s) (Nine Mile Point Ind. Estate, Cwmfelinfach, Gwent, UK), specifically comprising the Dynamometer (G100) and Pinchmeter (P100). The examination was conducted according to the recommendations of the American Society of Hand Therapists (ASHT). A standard test position includes a seated posture with feet flat, elbow flexed at 90°, and wrist and forearm in a neutral position.29, 30, 31 Three consecutive measurements were taken at 10-s intervals,30 and the average value obtained from these trials was considered the maximum grip strength. Depending on the child’s age, the dynamometer was set in 1 of the 5 standard test positions. The precision grip strength was assessed for 3 types of grips: Pincer, 3-point, and key (lateral). Results represent the mean of 3 measurements, expressed as a percentage of age- and gender-matched normative values32 and of the contralateral healthy hand. The results were evaluated according to the scoring system by Percival et al.33 and according to the hypoplastic thumb function assessment scale (WIMEC).34
The assessment of the hand’s manipulative-manual functions and how the thumb was used in daily activities was based on our developed test. The tasks in the test required using the hypoplastic thumb with lateral, 2-point, 3-point, and global grips. During the 1st trial, the patient was instructed to perform each activity in the manner most convenient for them. If a substitute grip was used, the patient was asked to retry lifting the object or performing the task using the hypoplastic thumb.
During the test, the order of task execution was arbitrary, the time for each task was unlimited, and the tasks included lifting and placing various objects:
1. Coin – lateral/2-point grip;
2. Sheet of paper – lateral/2-point grip;
3. Small round ball – 3-point, 2-point, small concentric grip;
4. Round plastic button – lateral, 2-point, 3-point grip;
5. Lifting a pen – 3-point grip;
6. Drawing a circle/line or drawing – 3-point grip;
7. Plastic block (cuboid) – global grip;
8. Bottle – global grip (large concentric);
9. and 10. Lifting a wooden peg and placing it into a hole, and then removing it and placing it back on the table.
For completing a task using the hypoplastic thumb, the patient received 1 point; for completing a task with a substitute grip and then in the subsequent trial using the thumb, 2 points; for completing a task only using a substitute grip, 3 points; and if the task was impossible to complete, 4 points. The scoring range was 10–40 points, with fewer points indicating a better outcome. The point score was also converted to a percentage scale of 0–100% task completion according to the following formula:
% total manual-manipulative ability = (40 − [total points scored])/30 × 100%.
Subjective hand function assessment was conducted using the Michigan Hand Outcomes Questionnaire (MHQ). Depending on the child’s age, the patient or the parent completed the test based on observations and conversations with the child. Because the test was initially designed for adults, the work module was modified to refer to school or household duties as work.
Additionally, an X-ray of the operated upper limb was performed during the check-up to assess the union of the transferred joint.
Results
The median passive range of motion for the hypoplastic thumb was 70° (range: 40–90°) at the interphalangeal (IP) joint, 35° (range: 5–45°) at the metacarpophalangeal (MP) joint, 75° (range: 30–90°) for radial abduction, and 70° (range: 10–90°) for palmar abduction. In 1 patient (No. 8), the first metacarpal was rigid with no passive motion; palmar and radial abduction measured 10° and 30°, respectively. Another patient (No. 7 after Huber opposition transfer) exhibited active palmar abduction up to 70° with an opposition strength of 4 on the Lovett scale. In 6 patients, opposition was possible to the tip of the little finger, and, in the remaining 2, to the tip of the long finger. In 6 cases (75%), there was an improvement in the stability of the hypoplastic thumb base; 1 case showed partial improvement (13%), and in 1 case, there was no improvement in stability.
The sensation in the pulp of the hypoplastic thumb among all the examined patients remained within normal limits, not exceeding 5 mm in the 2-point discrimination test (2PD) (Table 2).
The median of the AD/AB and AD/AC ratios, which determine the relative length of the thumb, were 49 and 25, respectively. Compared to the values established in the literature by Goldfarb et al., this indicates a 25% shorter relative thumb length.28
For global grip strength, the median value was 44% relative to the opposite healthy hand and 23% relative to the norm appropriate for the patient’s gender and age. Only 1 patient (No. 7) with active opposition after abductor digiti minimi muscle transfer could generate 2-point pinch strength, achieving 30% relative to the opposite healthy hand and 35% relative to the norm appropriate for the patient’s gender and age.
The manual manipulation function of the hand was assessed using our test for all the patients, with an average final score of 23 points. The total manual–manipulative ability ranged from 33% to 100%, with a median score of 55% for all the patients. The most difficult task was lifting small objects such as coins or small balls, and the least difficult was lifting larger objects such as a glass or block. Initially, 75% of the patients performed most of the tasks using a substitute grip and, then, in subsequent trials, used the hypoplastic thumb. However, half of the patients immediately used the hypoplastic thumb for some tasks. Two patients performed all the tasks immediately using the hypoplastic thumb, while 3 used only the substitute grip. During the study, most of the patients used a substitute grip at least once. The grip most commonly employed was the pinch between the index and middle fingers, used by over 60% of patients (Table 3).
Upon analyzing hand function according to the Percival scale, the most significant percentages of results were rated as fair (50%) and poor (37%). Only 1 result was rated as good (13%). The median score among the studied group was 13 points. Using the WIMEC, the median score was 22 points (range: 19–23) out of a max of 25.
Based on the subjective assessment of hand function using the MHQ, the median score for all the patients was 61%. The highest scores were noted in the sections on satisfaction and work, at 69% and 55%, respectively. The lowest scores were observed in the Activities of Daily Living (ADL) and esthetic section, at 47% and 54%, respectively (Table 4; Figure 2, Figure 3).
In 75% of cases, harvesting the PIP joint from the toe resulted in toe shortening, moderate in 5 patients and mild in 1 – though this did not pose a significant cosmetic concern. No patient experienced postoperative difficulties with ambulation or weight-bearing on the donor foot. However, 1 patient developed toe flaccidity after joint harvest, occasionally causing the toe to catch on footwear or when walking barefoot (Figure 4).
Only in 2 cases (25%) did the harvested graft not achieve union with the 1st or 2nd metacarpal bone after 8 weeks of immobilization with K-wires. In one case, infection around the Kirschner wires caused hardware instability; in another, wire loosening alone was responsible. Both cases necessitated reoperation: The first involved graft restabilization only, while the second required pseudoarthrosis resection, defect reconstruction with a bone graft, and subsequent restabilization. After surgery, union was achieved only in 1 patient, while pseudoarthrosis persisted in the other, resulting in ongoing thumb instability. In this case, the parents ultimately opted for pollicization (all the functional results of this patient presented in the paper refer to the assessment before the pollicization) (Table 5).
There was no statistically significant correlation between the age at surgery and relative thumb length with the manual manipulation function test (p = 0.256 and p = 0.417) or MHQ score (p = 0.923 and p = 0.493) (Table 6).
Discussion
According to the modified Blauth classification, thumb amputation followed by index finger pollicization is widely regarded as the gold-standard treatment for type III B thumb hypoplasia, delivering optimal functional outcomes.2 However, some parents decline this procedure due to concerns about its cosmetic effect, specifically, the resulting four-fingered hand. As a result, alternative reconstructive techniques aimed at preserving the hypoplastic thumb – with an emphasis on improving its stability, have been described in the literature. These reconstructive options include metatarsophalangeal (MTP) joint grafts (vascularized or non-vascularized), free phalanx grafts harvested from the toe, partial- or full-width metatarsal bone grafts, vascularized metatarsal transfers with full-thickness skin flaps, and non-vascularized structural grafts from the iliac crest.9, 10, 11, 14, 17, 18, 19, 23, 35, 36, 37, 38, 39
Autologous transfer of whole or partial PIP joints from the foot, using either vascularized or non-vascularized techniques, is well documented in both adult and pediatric populations as an alternative to arthrodesis or joint arthroplasty. Indications include congenital, traumatic, and post-infectious PIP joint deformities of the fingers.40, 41, 42
Kuzu et al.41 reported on 7 adult patients who underwent vascularized transfer of the second toe PIP joint to the hand, demonstrating enhanced joint mobility. After 1 year, passive range of motion improved by 5–53°, and active range by 2–43°. In a separate series, Dautel et al.40 evaluated 43 PIP joint reconstructions in children and adults over a 5-year follow-up, reporting a mean active range of 45° (range 34–79°). However, 2 transplanted joints developed complete ankyloses.
Our literature review revealed no reports of using a PIP joint transfer for type III B hypoplastic thumb reconstruction. However, some authors have described vascularized MTP joint grafts, with or without full-thickness skin flaps, as alternatives to pollicization.14, 18, 36 In these series, 10 patients aged 1–16 years underwent the procedure: For younger children, parents declined pollicization, while older patients received surgery solely to improve thumb stability in the absence of prior pollicization. In all cases, adjunctive tendon transfers were performed to restore active thumb motion. Postoperative thumb stability improved in all cases. However, only Matsuzaki et al.18 reported joint mobility, documenting radial abduction of up to 45° and palmar abduction of up to 75°. Some patients achieved global grip strength up to 3-fold higher, while key pinch strength remained 50% lower compared with pollicized individuals.36 In contrast, a separate study reported grip strength at 40% and 2-point pinch strength at 14% relative to the contralateral healthy hand.14 In 2 studies,18, 36 all the patients were able to grasp both small and large objects with the operated thumb, whereas, in the study by Foucher et al.,14 over half of the patients could grasp small objects with the hypoplastic thumb but only used this grip occasionally during daily activities, with most being able to hold larger objects.
Another technique described in the literature involves free, non-vascularized grafting of the entire or partial proximal phalanx or metatarsal bone from the foot to the base of the hypoplastic thumb.9, 10, 11, 17 A total of 40 patients across 4 studies were operated on at an average age of just under 2 years, with an average follow-up of over 5 years. In total, 60% of the patients had a diagnosis of type III B thumb hypoplasia, while the remaining had type IIIC or IV (5% and 35%, respectively). Most patients underwent tendon transfers tailored to their specific requirements, primarily opponensplasty. Good stability of the reconstructed CMC joint was achieved in most cases, although instability persisted in 2 patients10, 17 (1 after half-width metatarsal transfer and the other after phalanx transfer). In 1 case,17 partial instabilities were left uncorrected due to overall functional improvement.
In contrast, in another case,10 complete instability required reoperation with vascularized MTP joint transfer, which improved thumb stability and function. Only the study by Kawabata et al.17 evaluated the range of motion in the hypoplastic thumb, which averaged 35° of palmar abduction and 33° of radial abduction. The mean Kapandji score of all the patients was just under 6 points. All the studies assessed pinch grip strength, but only 39, 10, 17 compared it to that of the healthy contralateral hand, with an average strength of 31%. Chow et al.10 also evaluated global grip strength, which averaged 61% compared to that of the healthy contralateral hand. In 1 study, Goldfarb and Manschke’s method was used to compare the hypoplastic thumb’s length to the index finger’s proximal phalanx, finding it to be 57% of normal.17 Most of the evaluated patients9, 11, 17 could grasp smaller objects, though they more frequently used the hand for grasping larger objects. All the patients evaluated for donor site outcomes on the foot had no issues with walking, running, or weight-bearing, and shortening of the toe did not cause functional or cosmetic problems. The overall complication rate among all the patients was 18%. The most frequent complication was delayed or nonunion of the graft (four cases), with one instance each of donor-site mid-metatarsal fracture, fracture of the transferred metatarsal in the thumb, and first carpometacarpal (CMC I) joint instability. Based on 2 studies,9, 11 all the parents were postoperatively satisfied with the hypoplastic thumb’s function and appearance.
In our clinical evaluation, after stabilizing the hypoplastic thumb with a PIP joint from the foot, we achieved improved thumb stability and reduced hypermobility, consistent with the results reported in the abovementioned studies. Similar to Chow et al.,10 1 of our cases experienced persistent instability due to graft nonunion with the second metacarpal despite reoperation, ultimately necessitating pollicization.
Consistent with earlier reports, our patients were able to grasp large objects because the stabilized opposable thumb provided counterpressure against the other fingers during a global grip. However, grasping smaller objects was more challenging for most of our patients than in the studies mentioned above, likely due to limited active thumb movement, as only 1 patient underwent tendon transfers for thumb opposition. Due to the lack of object standardization across all studies, the results remain inconclusive.
We achieved results regarding the radial and palmar abduction range of motion similar to those for the patient in the study by Matsuzaki et al.18 and twice as good as those reported by Kawabata et al.17 The mean Kapandji score in our study was similar to that in the studies mentioned above, averaging just under 6 points. We obtained comparable global grip strength results, with a median of 44% compared to the contralateral healthy hand, as reported by Foucher et al.14 and Chow et al.,10 where the average results were 40% and 61%, respectively. The relative length of the hypoplastic thumb compared to the proximal phalanx of the index finger (according to the method developed by Goldfarb et al.28 was slightly more significant in our patients, measuring 72% compared to 57% in the study by Kawabata et al.17
In our study, only 1 patient (No. 7 after Huber opposition transfer) could generate 2-point pinch strength, likely due to the difficulty in overcoming the device’s resistance, as the other patients lacked active adduction and thumb opposition. In this patient, grip strength was 34% of the normative value, comparable to the 31% average reported in previous studies. Similarly to the studies cited, long-term follow-up showed that patients and their parents were satisfied with the surgical outcomes and would opt for the procedure again.
In our study, similarly to the study by Garagnani et al.,43 most patients had a shortened donor toe after the PIP graft was harvested. However, despite this, there were no significant functional foot issues or significant cosmetic concerns from either parents or patients.
The complication rate in our patient group was 25%, similar to the level reported in the reviewed studies (18%), with graft nonunion being the main issue, leading to CMC I joint instability. We performed reoperations in both cases, with union achieved in only 1, while instability persisted in the other, ultimately necessitating pollicization. In 1 case, graft nonunion resulted from infection around the Kirschner wires and subsequent hardware destabilization; in the other, nonunion was solely due to wire loosening. In the second case, despite graft restabilization, osseous union was not achieved. The patient presented with multiple congenital conditions, including thumb hypoplasia, congenital hearing loss, and hydrocephalus, which may have contributed to the nonunion. Ultimately, the parents consented to pollicization.
Our observations and the cited studies indicate that achieving improved thumb stability requires successful graft integration, regardless of the type of graft used.
If this surgical technique fails to achieve a satisfactory functional outcome for the patient, classical pollicization remains a viable option. In 1 of our cases, we performed pollicization with persistent thumb instability (during graft nonunion despite reoperation). We found no technical difficulties in performing pollicization as a secondary operation. No patient in our series required pollicization after achieving complete graft union, so we cannot directly assess this scenario. However, based on our experience, a prior successful graft union is unlikely to substantially alter the technical challenges or complication rates of subsequent pollicization.
In our work, we used the WIMEC scale to objectively assess the hypoplastic thumb function, a functional assessment score for congenital hypoplastic thumbs proposed by Mende et al. in 2021.34 It is a basic score, applicable even in young and non-cooperative patients. Because the WIMEC scale has been described only recently, it awaits proper validation and reliability testing. Utilizing this scoring system enables precise comparison of preoperative and postoperative status and facilitates benchmarking outcomes across different techniques and centers.44, 45 Currently, in the literature, only Sletten et al.45 have used WIMEC as one of the methods for an objective postoperative outcome. He assessed the stability of the thumb’s MP joint after ligament reconstruction with flexor digitorum superficialis in thumb hypoplasia type II and IIIA. Postoperatively, patients in the comparison groups achieved a mean WIMEC score of 30 points, surpassing our cohort’s median score of 22 points, likely reflecting their less severe thumb hypoplasia.
None of the studies reviewed employed either the Percival scoring system or the Michigan Hand Outcomes Questionnaire (MHQ), precluding direct comparison with our findings.
Limitations
The small patient group is a limitation of this study. Also, a detailed subsequent evaluation with long-term follow-up would be preferable. It will be valuable to compare the obtained results with those for patients after index pollicization as the gold standard for treating grade IIIB thumb hypoplasia.
Conclusions
Patients who underwent hypoplastic thumb reconstruction using a non-vascularized PIP joint graft from the foot experienced improved thumb stability and reduced hypermobility. These outcomes are comparable to those reported for similar reconstructive techniques in the literature. This method may be considered an option for stabilizing a hypoplastic thumb in patients whose parents do not consent to pollicization.
To achieve a better functional effect, it is necessary to plan the required tendon transfers for a given patient in 1 or more stages of treatment. The most important condition for success is the bone union of the graft, regardless of its type, because its failure is the most common complication, resulting in no improvement in thumb stability. Harvesting a PIP joint from a toe most often leads to shortening of the toe but does not cause gait disturbances or problems with weight bearing.
At follow-up, both patients and their parents reported satisfaction with the surgical outcomes and expressed willingness to undergo the procedure again. However, we emphasize that this technique is not intended to replace pollicization as the gold-standard treatment but should be reserved for cases in which parental consent for pollicization is not granted.
Data Availability Statement
Data sharing is not applicable to this article, as all data are already included in the manuscript.
Consent for publication
Not applicable
Use of AI and AI-assisted technology
Not applicable

















.jpg)
.jpg)
.jpg)
.jpg)