Abstract
Background. Septic shock in pediatric intensive care units (PICUs) requires accurate prognostic tools. The Sequential Organ Failure Assessment (SOFA) and the Phoenix Sepsis Score (PSS) are both widely used, yet their comparative effectiveness has not been fully established.
Objectives. To evaluate the prognostic sensitivity of the SOFA and PSS scores in predicting mortality among pediatric patients with septic shock, and to compare their performance across different patient subgroups.
Materials and methods. This retrospective study included 110 pediatric patients with septic shock admitted to the PICU of Shanxi Children’s Hospital between 2020 and 2024. SOFA and PSS scores were recorded at admission, along with demographic, clinical, and outcome data. Patients with congenital organ abnormalities or severe inherited metabolic disorders were excluded. Predictive accuracy was assessed using correlation analyses and receiver operating characteristic (ROC) curve analysis.
Results. Both SOFA and PSS scores showed moderate correlations with mortality (SOFA: r = 0.57; PSS: r = 0.56), with SOFA demonstrating slightly higher overall predictive accuracy. PSS exhibited greater sensitivity in severe cases. Neurological and respiratory dysfunctions were the strongest predictors of mortality, whereas coagulation parameters had minimal prognostic value. Age-specific analysis revealed that SOFA was more accurate in patients aged 1–3 years and >7 years, while PSS outperformed SOFA in children aged 3–6 years.
Conclusions. Both SOFA and PSS scores are effective tools for predicting mortality in pediatric septic shock. SOFA demonstrated superior overall performance, whereas PSS showed advantages in specific age ranges and disease categories. Using the two scoring systems in combination may support more informed clinical decision-making.
Key words: SOFA score, pediatric septic shock, PSS score, prognostic evaluation, scoring system comparison
Background
Septic shock is one of the most critical and life-threatening conditions commonly encountered in pediatric intensive care units (PICUs), with a high incidence and mortality rate.1, 2 Accurate assessment of disease severity and prediction of mortality risk are essential for formulating appropriate treatment strategies and improving patient outcomes. However, predicting outcomes in pediatric septic shock remains a major clinical challenge due to heterogeneous presentations, rapidly evolving physiology, and varied responses to treatment.
Currently, various scoring systems are used in clinical practice to evaluate the severity of septic shock.3, 4, 5 Among them, the Sequential Organ Failure Assessment (SOFA) score and the Phoenix Sepsis Score (PSS) are key tools for diagnosing pediatric sepsis.6, 7 The SOFA score quantifies organ dysfunction by evaluating multiple organ systems, including respiratory, circulatory, hepatic, coagulation, neurological, and renal functions, making it a general-purpose tool originally developed for adults.8 In contrast, the PSS score is specifically designed for pediatric patients, focusing on indicators relevant to pediatric physiology to predict mortality risk.7 It is a recently developed, pediatric-specific scoring system that incorporates age-adjusted physiological and clinical parameters tailored to pediatric patients’ unique pathophysiology.9
Despite their widespread use, few studies have directly compared SOFA and PSS in pediatric septic shock, especially in terms of predictive accuracy across different age groups and disease categories.10 Existing literature either focuses on adult populations or evaluates these tools independently, without highlighting how their structures and clinical applications differ. While SOFA provides a broad overview of organ failure, PSS integrates pediatric-specific variables, potentially offering better sensitivity in younger age groups.11 This gap in comparative evidence limits clinicians’ ability to choose the most effective prognostic tool in pediatric settings.
With the implementation of the 2024 International Consensus Criteria for Pediatric Sepsis and Septic Shock, the PSS has superseded the prior diagnostic criteria based on systemic inflammatory response syndrome (SIRS).7 This new scoring system was created by a group of 35 pediatric experts from 6 continents, using data from international surveys, systematic reviews, meta-analyses, and a comprehensive dataset of over 3 million electronic health records from 10 sites on 4 continents.1 Since the PSS has only recently been adopted, its comparative utility relative to established scoring systems such as SOFA remains insufficiently studied, especially in real-world PICU settings.
This study examines previously collected data from pediatric patients with septic shock who were treated in the PICU at Shanxi Children’s Hospital, China between January 1, 2020, and December 31, 2024. It attempts to assess how well the SOFA and PSS scores predict the risk of mortality and which score is better at identifying individuals at higher risk. The study also looks at how different aspects of each grading system influence patient outcomes and analyzes their accuracy across disease categories. To our knowledge, this is one of the first studies to directly compare SOFA and the newly implemented PSS in a pediatric septic shock cohort, filling a critical evidence gap and providing practical insights to enhance risk stratification in clinical care.
Objectives
This study compared the ability of SOFA and PSS scores to predict death in pediatric septic shock and discovered which is more sensitive in identifying high-risk individuals. It also investigated how individual components of each score contribute to death prediction and compared their effectiveness across disease categories.
Materials and methods
Study population
This study comprised pediatric patients diagnosed with septic shock who were admitted to Shanxi Children’s Hospital’s Pediatric Intensive Care Unit between January 1, 2020, and December 31, 2024. Patient selection was conducted retrospectively by reviewing electronic medical records.
Inclusion criteria were as follows: 1) patients meeting internationally recognized diagnostic criteria for pediatric septic shock;12 2) patients who underwent SOFA and PSS scoring immediately upon PICU admission, with all relevant subcomponent data recorded; and 3) patients with complete clinical records, including all required physiological and laboratory parameters to calculate both SOFA and PSS scores, as well as outcome data.
Exclusion criteria were as follows: 1) Patients with severe congenital organ malformations or uncontrolled severe inherited metabolic disorders; 2) Patients who had undergone major surgery or prolonged intensive care treatment prior to admission; 3) Patients with missing, incomplete, or inconsistent medical records that would prevent accurate SOFA or PSS scoring.
Patients with partially missing data were excluded only if the missing elements affected score computation. Otherwise, such cases were retained, and missing values were managed via cross-validation with laboratory and clinical notes.
This study was approved by the Institutional Review Board of Shanxi Bethune Hospital (approval No. IRB-WZ-2025-009).
Data collection
The following data were collected for each patient: general demographic information (age, sex, and disease category), disease-related information (diagnosis), and SOFA and PSS scores upon admission. The SOFA score included subcomponents for respiratory, coagulation, hepatic, circulatory, neurological, and renal function, whereas the PSS score included respiratory, circulatory (cardiovascular and mean arterial pressure), coagulation, and neurological function. Additionally, the final outcome (survival or death) within 72 h of PICU admission was recorded.
All SOFA and PSS scores were calculated retrospectively by 2 trained pediatric intensive care physicians working independently. To assess inter-observer variability, a random subset of 20 patient records was scored by both physicians. The inter-rater reliability was evaluated using the intraclass correlation coefficient (ICC), and discrepancies were resolved by consensus.
Scoring methods
The SOFA scoring system assesses 6 organ systems: respiratory, coagulation, hepatic, circulatory, neurological, and renal function. Each system is scored based on specific physiological indicators and laboratory test results, with a total score ranging from 0 to 24. Higher scores indicate greater severity of organ dysfunction.
The PSS scoring system is based on the 2024 International Consensus Criteria for Pediatric Sepsis and Septic Shock. It evaluates respiratory, circulatory, coagulation, and neurological functions to estimate the risk of death in pediatric patients.
Statistical analyses
Sample size justification
A total of 110 patients were included, based on the availability of complete and valid clinical data collected between 2020 and 2024. This sample size was considered adequate for exploratory analysis and subgroup comparisons, given the rarity and high-risk nature of pediatric septic shock.
Comparison of SOFA and PSS scores in predicting 72-hour mortality
Python software (https://www.python.org/) was used to analyze how well SOFA and PSS scores predict mortality. The point-biserial correlation coefficient was applied because the outcome variable (survival vs death) was binary. The predictive performance of both scoring systems was compared by examining the absolute values of their correlation coefficients, where higher values indicated stronger predictive accuracy.
We used Python to calculate Pearson’s correlation coefficients to assess how each SOFA subcomponent relates to mortality. A coefficient with an absolute value closer to 1 signified a stronger association with patient outcomes. The significance of the correlation was evaluated using the p-value, with p < 0.05 considered statistically significant. Pearson’s correlation coefficients and p-values were calculated for each PSS subcomponent to assess their association with mortality outcomes.
Patients were categorized into 4 age groups: <1 year, 1–3 years (including 3 years), 3–7 years (including 7 years), and >7 years. The distribution of patients in each group is shown in Supplementary Table 1. Python was used to calculate the impact of SOFA and PSS scores on mortality outcomes within each age group.
Using Python, we analyzed total SOFA and PSS scores by disease category, excluding the miscellaneous and Kawasaki disease groups, to evaluate their predictive performance for mortality. Sensitivity was calculated, and hypothesis testing was conducted to determine whether there was a significant difference between the 2 scoring systems in mortality prediction.
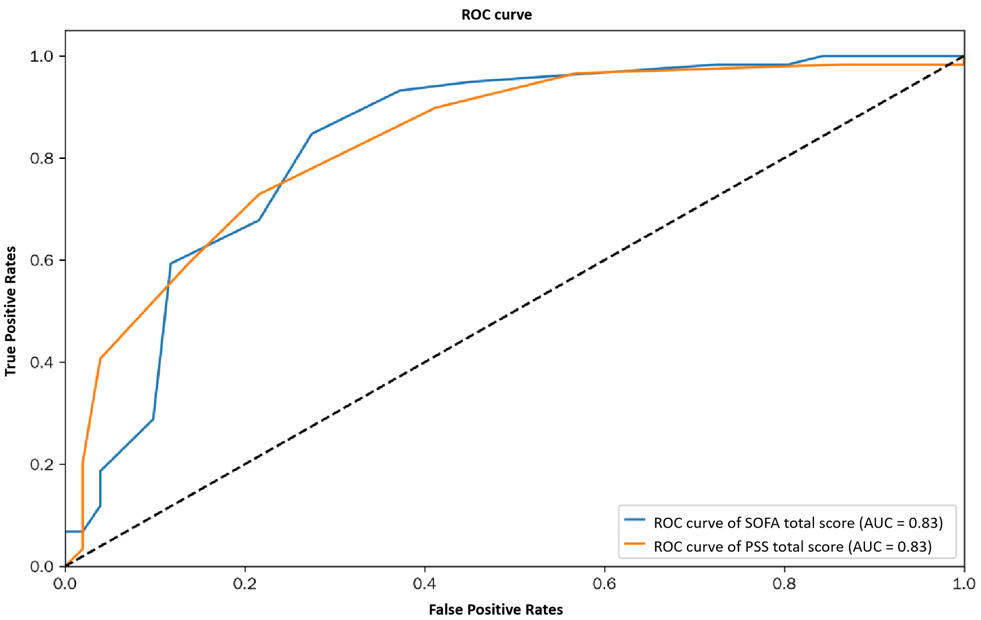
Receiver operating characteristic curves were generated using Python to determine the optimal thresholds for the 2 scoring systems (Figure 1). Exceeding these thresholds is linked to a substantially higher risk of mortality.
Results
The prognostic accuracy of the SOFA and PSS scores in predicting mortality among pediatric patients with septic shock in the PICU was assessed. We used correlation analysis, true positive rate (TPR) calculations, and subgroup analyses to evaluate their performance.
Overall correlation with mortality
As shown in Table 1, the SOFA score had a correlation coefficient of 0.57 with mortality, which falls into the category of a moderate positive correlation (defined as 0.4 ≤ r < 0.7). This suggests that higher SOFA scores were linked to an increased risk of death. The correlation was statistically significant, with a p-value of 7.04 × 10–11, well below the standard 0.05 threshold. Similarly, the PSS score showed a moderate positive correlation with mortality (r = 0.56, p = 2.26 × 10–10), also confirming a significant association. A direct comparison of these values revealed that the SOFA score had a slightly stronger correlation with mortality than the PSS score, though the difference was minimal in predicting outcomes within 72 h of PICU admission.
True positive rate performance
Table 2 provides further insights into the predictive performance of both scoring systems. The TPR analysis showed that higher SOFA scores were associated with an increased likelihood of correctly identifying non-survivors. This trend suggests that higher SOFA scores were associated with more accurate mortality predictions. In particular, in the highest score range (13.667, 15.333), the TPR reached 0.875, suggesting strong predictive accuracy. The PSS score exhibited a similar trend in Table 3, with higher score intervals corresponding to increased TPR. Notably, the highest TPR for the PSS score was 0.923 in the (7.778, 8.889) and (8.889, 10.0) range, surpassing the TPR of the SOFA score in most intervals. This indicates that while both scoring systems were effective in identifying high-risk patients, the PSS score demonstrated slightly higher sensitivity in predicting mortality, particularly in the highest score ranges.
Subcomponent analysis
In Table 4, subcomponent analysis revealed that among the SOFA score components, the nervous system and respiratory sub-scores had the highest correlation with mortality, with correlation coefficients of 0.447 and 0.447, respectively. These findings indicate that neurological and respiratory dysfunctions were the most critical factors influencing patient outcomes in septic shock cases. The circulatory sub-score had a weaker but still significant correlation with mortality (0.317, p < 0.05), while the renal sub-score (0.203, p = 0.033) showed a marginally significant relationship. The hepatic and coagulation sub-scores, however, had lower correlation coefficients and p-values above 0.05, suggesting that their impact on mortality was not statistically significant.
For the PSS score subcomponents in Table 5, the respiratory sub-score demonstrated the strongest association with mortality, with a correlation coefficient of 0.460and a highly significant p-value (4.359 × 10−7). The nervous system and cardiovascular sub-scores also had significant positive correlations with mortality (0.407229 and 0.391132, respectively, p < 0.05), reinforcing the importance of these physiological systems in predicting patient outcomes. The circulatory mean arterial pressure (MAP) sub-score (0.321, p < 0.05) exhibited a weaker but still significant relationship with mortality. In contrast, the coagulation sub-score showed no significant correlation with mortality, with a coefficient of only 0.029 and a p-value of 0.765, indicating its minimal contribution to prognosis.
Age-stratified performance
Age-stratified analysis of predictive sensitivity in Table 6 revealed that the performance of the SOFA and PSS scores varied across different pediatric age groups. In patients aged 1–3 years, the SOFA score demonstrated higher sensitivity (0.688) compared to the PSS score (0.625), indicating better predictive ability for mortality in this subgroup. Conversely, in patients younger than 1 year, the PSS score exhibited greater sensitivity (0.733) than the SOFA score (0.600), suggesting that the PSS score was more effective in predicting mortality for this age group. In pediatric patients aged 3–7 years, the PSS score had higher sensitivity (0.750) compared to the SOFA score (0.625). However, in pediatric patients older than 7 years, the SOFA score (0.750) outperformed the PSS score (0.667). This demonstrates that the accuracy of both scoring systems varies by age, with SOFA being more accurate in older pediatric patients and PSS doing better in younger ones.
A χ2 test was used to determine the relationship between SOFA and PSS scores and mortality in various age groups. The analysis compared the median values of both scores, which are displayed in Table 7. A p < 0.05 was judged statistically significant. The findings demonstrated that the accuracy of these scores varies with age. As a result, when applying these scores in clinical practice, age must be taken into account.
Overall, both SOFA and PSS scores were strongly related to death in pediatric septic shock patients, with SOFA performing marginally better in prediction. However, PSS was more sensitive in patients at higher risk, particularly in younger pediatric patients. According to subcomponent analysis, neurological and respiratory dysfunctions have the greatest impact on patient outcomes. Age-stratified analysis underlined the significance of tailoring the usage of these scores to the patient’s age.
The usefulness of SOFA and PSS in predicting death differed by age group. The SOFA score in pediatric patients aged 1–3 years had a p-value of 0.056, which was somewhat higher than the 0.05 significance level. This indicated that its predictive value in this population was not statistically significant. On the other hand, the PSS score had a p-value of 0.012, showing a significant association with mortality. In infants under 1 year old, both SOFA (p = 0.031) and PSS (p = 0.015) scores revealed clear relationships with mortality risk. Similarly, in the 3–7 year age group, both scores were substantially linked with mortality, with the PSS score (p = 0.001) having a larger connection than the SOFA score (p = 0.018). Among pediatric patients older than 7 years, the SOFA score (p = 0.019) remained a significant predictor of mortality, whereas the PSS score (p = 0.054) was just above the statistical threshold, suggesting a weaker association. These findings highlight that the predictive performance of the SOFA and PSS scores varies by age, with PSS being more effective in younger pediatric patients and SOFA demonstrating better accuracy in older age groups.
Disease-specific sensitivity analysis
The study cohort included patients diagnosed with respiratory diseases, digestive system diseases, postoperative gastrointestinal conditions, neurological disorders, and hematologic diseases. Sensitivity analysis (Table 8) evaluated how well the SOFA and PSS scores predicted mortality across these conditions. The SOFA score showed higher sensitivity (0.818) in respiratory diseases compared to the PSS score (0.636), indicating a stronger predictive ability in this category. However, in digestive system diseases, the PSS score (0.778) outperformed SOFA (0.667), suggesting better mortality prediction for these patients. For postoperative gastrointestinal conditions, SOFA (0.889) again had higher sensitivity than PSS (0.778), indicating its superior ability to assess mortality risk after surgery. Among patients with neurological disorders, the PSS score (0.600) was more effective than the SOFA score (0.333), suggesting stronger predictive power in this group. In hematologic diseases, both scores showed equal sensitivity (0.444), meaning their predictive accuracy was comparable. The McNemar’s test (Table 9) found no statistically significant differences (p > 0.05) between the 2 scoring systems across these disease categories, indicating that while they differ in sensitivity for specific conditions, both provide valuable clinical insights without major disparities in overall predictive accuracy.
Threshold and ROC curve analysis
Threshold analysis (Figure 1) identified critical score cutoffs for assessing mortality risk. A SOFA score above 10 was associated with a significantly increased risk of mortality, while a PSS score exceeding 6 also indicated a substantially elevated risk. These criteria are useful clinical reference points for determining the severity of pediatric septic shock. Using Youden’s index method, the study determined ideal cutoff values (Table 10) to aid in the differentiation of survivors and non-survivors across disease groups. These findings provide clinicians with a crucial tool for making early decisions and assessing risks in critically unwell pediatric patients.
We utilized receiver operating characteristic (ROC) curve analysis to determine how effectively SOFA and PSS scores predicted mortality across illness categories (Figure 2). In respiratory illnesses, the SOFA score had a greater AUC value. This suggested that it was more accurate in mortality prediction than the PSS score, which was still effective but significantly less precise. For digestive system illnesses, the SOFA score exhibited a somewhat lower balance of true and false positive rates, although both scores are still effective.
While the PSS score was equally useful but had a somewhat lower area under the curve (AUC) value, the SOFA score showed high prognostic ability in postoperative gastrointestinal problems. Both scores were helpful in determining mortality risk in neurological illnesses, although PSS outperformed SOFA. The PSS score had a marginally higher AUC value for hematologic disorders. In this category, the PSS score was therefore the more accurate predictor.
Overall, the SOFA score tended to produce ROC curves closer to the upper left corner, indicating better overall performance for mortality prediction. However, the PSS score consistently performed better than random chance and remained a useful method for assessing risk. These differences show the importance of opting for the most suitable scoring system based on patient’s condition, so as to improve risk assessment and clinical decisions.
This study offers a detailed comparison of the SOFA and PSS scores in mortality prediction among pediatric septic shock patients. The results show that their accuracy depends on age and type of disease. The SOFA score was generally more effective for respiratory and postoperative gastrointestinal conditions. The PSS score was more effective for digestive system diseases and neurological disorders. The identification of threshold values in this study provides practical guidance for clinical risk assessment. Both scoring systems are valuable for disease severity evaluation, but their different strengths across subgroups show the need for a customized approach to patient management.
Discussion
Pediatric septic shock continues to present high mortality rates.13 The disease can progress rapidly, and clinicians often lack objective tools for timely assessment.14, 15 The SOFA score has been adapted for pediatric use and is already applied in some clinical settings.16 The introduction of the PSS in 2024 has broadened perspectives and has been practically applied, yet challenges persist in its usage.17 Both scoring systems have their respective merits, and their superiority remains inconclusive. This study conducts a preliminary comparative analysis of the 2 scoring systems based on collected data, aiming to identify potential issues and provoke further reflection.
The findings confirm that higher SOFA and PSS scores are associated with increased mortality risk, consistent with known disease progression patterns. This reinforces both systems as valuable tools for initial risk stratification. However, mortality in low-scoring cases highlights the rapid progression of septic shock, where patients can deteriorate within a short period.18 Lower-scoring cases tend to receive less attention compared to higher-scoring cases. Dynamic scoring at multiple time points, combined with the integration of real-time biomarkers such as B-type natriuretic peptide (BNP) and cardiac enzymes, may enhance early detection and improve risk prediction.19, 20, 21
The SOFA score has limitations when applied to children, as physiological parameters vary significantly across different pediatric age groups compared to adults.22, 23 For example, in the cardiovascular system assessment, the SOFA score categorizes MAP at a threshold of 70 mm Hg, which is not accurate for children. Before the introduction of the PSS score, modifications to the SOFA score were attempted to accommodate pediatric physiological characteristics,16, 24 but these adaptations were not widely adopted. In pediatric practice, vasoactive medication use is often utilized for scoring pediatric septic shock patients.25, 26 However, this method may overlook pediatric patients with a tendency for hypotension who have not yet received vasoactive medications, necessitating experienced clinicians to remain vigilant. The PSS builds on this approach by incorporating age-specific criteria.21 Nevertheless, the MAP criteria in PSS remain stringent. Among all cases collected in this study, only 19 patients received a score ≥1 for MAP, with only 8 scoring 2, despite 59 mortality cases. In deceased patients, cardiovascular system scoring was relatively more objective than MAP-based scoring. While MAP scoring is significantly correlated with mortality, its stringent thresholds result in fewer qualifying patients, limiting its practical utility in cases of rapid disease progression and underestimating severity.
The PSS score omits liver and renal function assessments compared to the SOFA score, making it more convenient in clinical applications. Notably, PSS introduces the SpO2/FiO2 (S/F) ratio as a respiratory assessment parameter, providing a reliable evaluation method for hospitals without mechanical ventilation facilities.7 This study found that liver and renal function assessments had a weaker predictive value for mortality, suggesting that PSS offers a more efficient approach. The evaluation of liver and kidney function often experiences delays, as it depends on laboratory tests. Given the rapid disease progression in critically ill pediatric patients, any delays in scoring could introduce biases in disease assessment. The PSS may offer a more time-efficient scoring system in emergency settings,27 while the SOFA score’s broader organ evaluation may offer advantages in complex or multi-system involvement.28
The age-dependent differences in mortality prediction between the 2 scoring systems present an interesting finding. In patients aged 1–3 years, the PSS score demonstrated superior predictive accuracy, whereas the SOFA score performed better in patients older than 7 years. Pediatric patients aged 1–3 years undergo rapid physiological changes and development,29 and the PSS score, which accounts for pediatric physiology, may thus offer more accurate predictions in this group. In contrast, pediatric patients older than 7 years exhibit physiological parameters closer to adult levels, diminishing the advantages of the PSS score compared to SOFA. However, in pediatric patients younger than 1 year and those aged 3–7 years, no significant differences were observed between the 2 scoring systems. This could be attributed to the relatively small sample size, highlighting the need for further research with larger datasets. It may also reflect developmental physiology, as older children resemble adult profiles where SOFA parameters are more applicable, whereas PSS’s pediatric-specific thresholds provide greater sensitivity in younger age groups.29 For instance, infants under 1 year primarily undergo physical and neurological development, while the respiratory and cardiovascular systems remain relatively stable. Similarly, pediatric patients aged 3–7 experience slower growth, with minimal fluctuations in physiological parameters. Our findings are consistent with earlier studies suggesting that developmentally aligned tools enhance prediction accuracy in young patients.29 These factors may contribute to the minimal differences observed between the 2 scoring systems in these age groups. Further interdisciplinary exploration with developmental experts is warranted to refine these findings.
The performance of these 2 scoring systems varies slightly across different disease categories. Due to the limitations of the cases collected in this study, we primarily compared diseases of the respiratory, digestive, nervous, and hematologic systems. Our findings indicate that for patients with respiratory diseases, digestive diseases, and post-digestive tract surgery, the SOFA score outperforms the PSS score in mortality prediction. However, for neurological and hematologic diseases, the SOFA score is slightly less effective than the PSS score in predicting mortality. This discrepancy may be attributed to differences in the focus of each scoring system. The SOFA score emphasizes the overall assessment of multiple vital organs, whereas the PSS score primarily evaluates 4 key aspects: respiration, circulation, neurological function, and coagulation. In the context of this study, which focuses on pediatric septic shock, both scoring systems assign relatively high weights to the circulatory system. However, in pediatric patients with respiratory diseases, the respiratory system is often the first to be affected and may suffer the most severe impairment. As both scoring systems assign significant numerical values to respiratory dysfunction, the key difference lies in the assessment of other organ systems. The PSS score is relatively less comprehensive in evaluating these systems compared to the SOFA score, which may explain why the SOFA score exhibits higher sensitivity in predicting mortality for respiratory diseases.
For patients with digestive diseases or post-digestive tract surgery, the presence of both digestive tract involvement and shock may lead to severe disturbances in fluid-electrolyte balance and acid-base homeostasis,30, 31 potentially affecting the stability of the respiratory, neurological, and urinary systems. The SOFA score provides a more detailed assessment of the neurological and urinary systems than the PSS score, which likely accounts for its higher sensitivity in predicting mortality in these disease categories.
For neurological diseases, the PSS score classifies patients into broader categories, whereas the SOFA score offers a more detailed breakdown. As a result, the SOFA score is slightly more sensitive in predicting mortality for neurological conditions.
Compared to other illness types, both scores are less sensitive in predicting mortality in hematologic diseases. This implies that neither score is suitable for this patient population. As a result, hematologic problems require a more sophisticated system.
There are distinct trends in the mortality thresholds for PSS and SOFA scores. The SOFA score threshold is close to the median value of the overall score distribution. This suggests that it serves as a more reliable indicator of disease severity. Significant organ dysfunction and an increased risk of death are indicated when a patient’s SOFA score is above this threshold. The PSS score, on the other hand, only substantially predicts mortality risk at higher levels; however, it also has a greater true positive rate within this range. This implies that the SOFA score is better for the slow and ongoing evaluation of illness progression, whereas the PSS score is better for identifying the most serious cases. This could explain SOFA’s advantage in multi-organ dysfunction scenarios such as post-surgical shock, while PSS is more sensitive to localized dysfunctions.
Variability in management practices also affects patient outcomes. Variability in antibiotic choice, timing of vasoactive drug use, and supportive therapies may all impact patient prognosis.32, 33 Standardized care pathways and clearer scoring-based treatment thresholds could reduce this variation and improve outcomes.
In contrast to our results, previous studies have found conflicting trends. A previous study suggested that PSS had superior overall accuracy in a neonatal population,34 whereas our data favors SOFA in older pediatric patients. This difference may be due to cohort variations, different inclusion criteria, or scoring implementation timing. These inconsistencies emphasize the need for multicenter validation across broader demographics.
These findings have important real-world implications. In emergency settings, the simplicity of the PSS and its reliance on fewer laboratory results make it particularly suitable for rapid triage.35 SOFA, while more comprehensive, may better guide long-term ICU management or therapy escalation decisions.36 Clinicians should consider using both scores complementarily – PSS for early warning and SOFA for monitoring disease trajectory.
Future directions should explore how treatment decisions (e.g., antibiotic initiation, ventilation, vasoactive support) correlate with score thresholds. Additionally, monitoring score trends over time could refine intervention strategies. For instance, rising scores may indicate the need for escalation, while declines could guide de-escalation. Artificial intelligence (AI) tools and wearable monitors could further personalize care, integrating real-time score updates into decision-making.
In summary, SOFA and PSS are both effective mortality predictors, each with distinct advantages. SOFA offers better overall performance, while PSS excels in early detection for certain age and disease groups. Their combined use may enhance prognostic accuracy and clinical decision-making. Further multicenter studies, score adaptations, and AI integration will be vital to optimizing care for pediatric septic shock.
Limitations
This study has notable limitations. One significant constraint is the relatively small sample size, limiting the collection of cases across different disease categories. For instance, there were a few cases of immunological and urinary system diseases complicated by septic shock, and no cases of inherited metabolic disorders with septic shock were included. These omissions may introduce potential bias. Given the limitations of cases available at our hospital and our current research capacity, future efforts should focus on collecting a more comprehensive dataset to facilitate further investigations. This remains an intriguing area of research.
Conclusions
The central finding confirms that both SOFA and PSS scores are effective in predicting mortality, with SOFA exhibiting a slightly superior overall performance (correlation coefficient = 0.57 vs 0.56). While the difference in predictive strength was modest, SOFA’s higher correlation and ROC performance (especially in respiratory and postoperative gastrointestinal cases) suggest it should be prioritized for general assessment and in patients aged 1–3 years and over 7 years.
However, PSS showed better sensitivity in high-score ranges and superior performance in patients younger than 1 year, pediatric patients aged 3–7 years, and in cases involving digestive and hematologic diseases. Specifically, PSS’s respiratory sub-score (r = 0.460) was the most predictive component, while coagulation factors had minimal prognostic impact in both systems. Neurological and respiratory dysfunctions emerged as the strongest mortality predictors within the SOFA framework.
For clinical practice, we recommend using the SOFA score as the primary tool for general prognostic assessment in pediatric septic shock, particularly in respiratory or surgical gastrointestinal cases, and among patients aged 1–3 and >7 years. Conversely, the PSS score should be prioritized in infants and in patients presenting with digestive or hematologic conditions.
Their combined application may offer complementary insights and enhance decision-making accuracy in age- and disease-specific contexts. Future studies are encouraged to further refine scoring models for improved specificity and broader applicability across diverse pediatric subpopulations.
Data Availability
The raw data supporting the findings of this study are openly available in Zenodo under separate links. The raw data can be accessed at https://doi.org/10.5281/zenodo.
15081539.
Supplementary data
The supplementary materials are available at https://doi.org/10.5281/zenodo.15833612. The package includes the following files:
Supplementary Table 1 Distribution of patients across different age groups.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.