Abstract
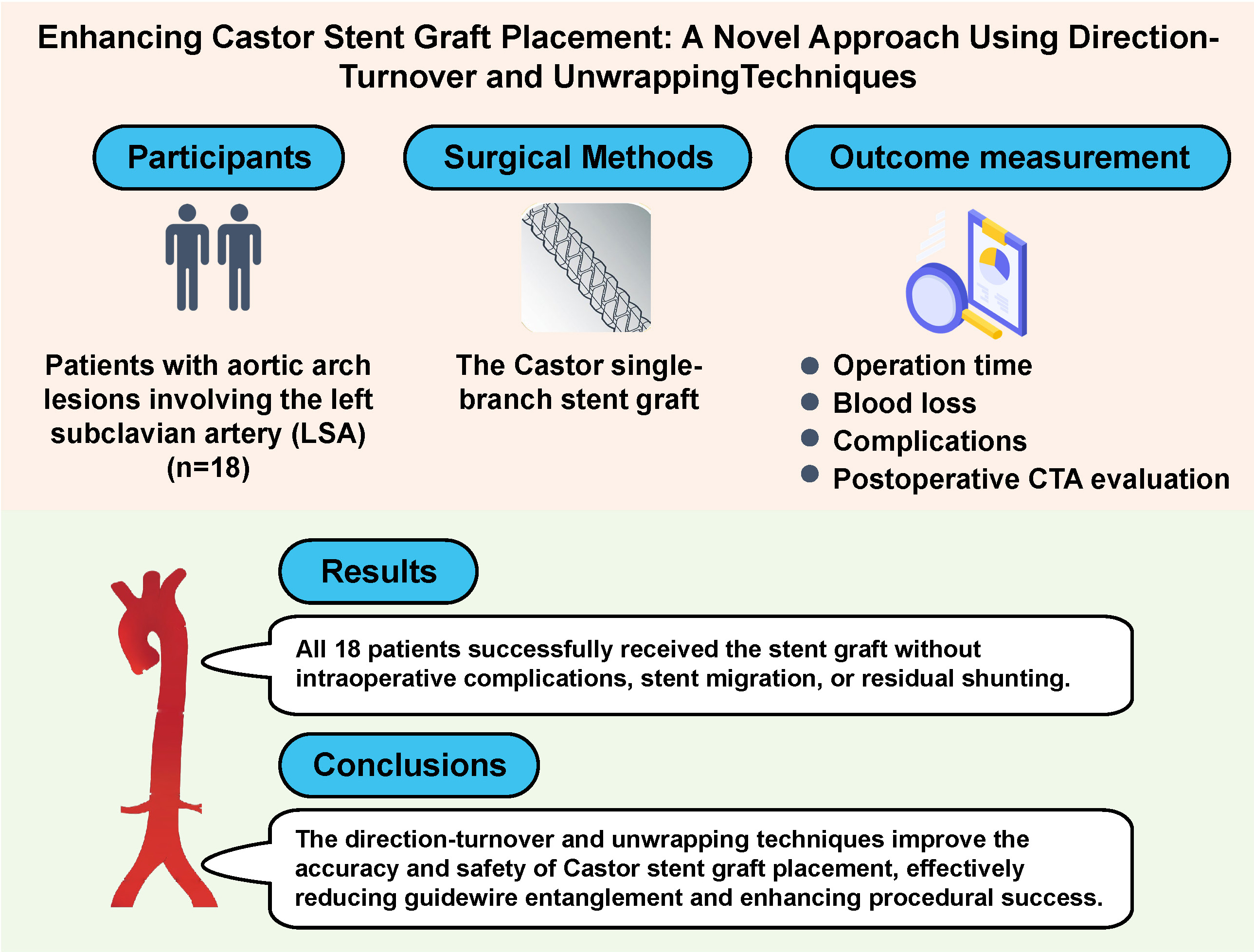
Background. Patients with aortic arch lesions involving the left subclavian artery (LSA) usually require endovascular surgery. The Castor single-branch stent graft provides a targeted solution for such cases, with potential benefits enhanced by the direction-turnover and unwrapping techniques.
Objectives. To evaluate the safety, efficacy and short-term outcomes of the direction-turnover joint unwrapping techniques combined with a Castor single-branch stent graft in treating aortic arch lesions involving the LSA.
Materials and methods. From January 2022 to June 2023, 18 patients with aortic arch and LSA lesions underwent Castor stent graft placement at Binzhou Medical University Hospital (Shangdong, China). Preoperative and postoperative imaging with computed tomography angiography (CTA) was used to assess stent placement and efficacy at 1, 3, 6, and 12 months post-surgery.
Results. All 18 patients successfully received the stent graft without intraoperative complications, stent migration or residual shunting. Postoperative imaging confirmed accurate stent placement with no evidence of thrombosis or endoleaks.
Conclusions. The direction-turnover and unwrapping techniques improve the accuracy and safety of Castor stent graft placement, effectively reducing guidewire entanglement and enhancing procedural success. These techniques show promise for broader application in complex aortic arch interventions.
Key words: Castor stent graft, direction-turnover, unwrapping, aortic arch lesions, left subclavian art
Background
Aortic arch diseases, which include aortic dissection, intramural hematoma, penetrating aortic ulcer, traumatic aortic disconnection, aneurysm, and aortic coarctation, pose significant health risks. The global incidence of aortic dissection alone is estimated at 2.8–6.0 cases per 100,000 individuals per year, with mortality rates reaching 50% within 72 h if untreated.1, 2 Similarly, aortic aneurysms have an annual incidence of approx. 5.9 per 100,000, with rupture cases demonstrating mortality rates as high as 90%.3 These diseases, particularly acute aortic syndromes such as aortic dissection and aneurysm rupture, are characterized by rapid onset, poor prognosis and high mortality, underscoring the need for prompt and effective treatment.
Traditionally, these conditions are treated with open thoracotomy and artificial vascular replacement of the aortic arch, procedures that require general anesthesia and hypothermic cardiopulmonary bypass. However, this approach has significant limitations; it is not suitable for elderly patients or those with underlying health conditions, as hypothermic cardiopulmonary bypass can lead to ischemia/reperfusion (I/R) injuries in the heart and brain. In 1994, Dake et al.4 introduced thoracic endovascular aortic repair (TEVAR) as a less invasive alternative to open thoracic aortic surgery, utilizing catheter-based techniques within the aortic lumen under imaging guidance.5 Compared to open and hybrid surgeries, TEVAR offers advantages of reduced trauma, lower risk of complications, better aesthetics outcomes, and favorable prognosis.
However, single-graft TEVAR alone cannot adequately address complex aortic arch diseases, particularly when branch artery reconstruction is necessary.6 To address this, new methods have emerged, including the chimney,7 in situ fenestration,8 in-situ fenestration,9 and branched stent techniques.10 Each approach offers unique benefits but also presents distinct limitations. The chimney technique, for instance, involves placing a secondary “chimney” stent alongside the primary graft to maintain blood flow to vital arteries. However, this approach is prone to type I endoleak, as the primary stent graft often has incomplete adhesion to both the chimney graft and the aortic wall.11 The in situ fenestration technique enables direct creation of fenestrations in the graft within the patient’s body but poses a high risk of vascular damage from the needle or laser used.12 Finally, while the branched stent technique reduces the risk of endoleak, its technical complexity can limit its use.13 Despite improvements in design and deployment methods, these approaches still face limitations in widespread clinical adoption.
The Castor single-branch stent (Figure 1) was developed to provide a solution tailored to complex aortic arch pathologies. Jointly developed by Shanghai Changhai Hospital and Shanghai Endovastec Company, the Castor stent received regulatory approval in 201714 and has been used in over 5,000 cases as of June 2021.15 Its single-branch design facilitates the reconstruction of left subclavian artery (LSA) blood flow, improving stent anchoring and stability. Additionally, the proximal “fenestration” enables blood flow to the left common carotid and infracarotid arteries, allowing partial reconstruction of aortic arch branches. These features make the Castor stent a promising approach in managing aortic arch diseases that require both stability and preservation of branch artery blood flow.16
In this study, we further enhanced the application of the Castor stent by introducing direction-turnover and unwrapping techniques. These methods were developed specifically to address the challenges of graft positioning and operational complexity in complex aortic arch reconstructions. The direction-turnover technique utilizes spatial inversion to ensure accurate alignment of the stent fenestration with the aortic arch branches, improving placement precision. Meanwhile, the unwrapping technique mitigates the risk of guidewire entanglement, facilitating a smoother and safer procedure. Together, these techniques enhance procedural efficiency and safety, making the Castor stent a more effective solution for complex aortic arch repairs.
Objectives
The aim of the study was to evaluate the safety, efficacy and prognosis of using the directional turning and unwrapping techniques with the Castor single-branch stent graft in the treatment of lesions of the aortic arch and left subclavian artery based on clinical data and follow-up results from 18 patients.
Materials and methods
Participants
A total of 18 patients with aortic arch disease involving the LSA were successfully treated with a Castor single-branch stent graft in Binzhou Medical University Hospital (Shangdong, China). This cohort included 17 men (94.4%) and 1 woman (5.6%), with an average age of 58.72 ±11.28 years. The demographic and clinical data are presented in Table 1, Table 2, Table 3. Written informed consent was obtained from the participants prior to the enrollment of this study.
Inclusion criteria: 1. Patients presented with clinical symptoms of aortic arch disease, such as chest pain and tightness. 2. Aortic arch disease was confirmed using computed tomography angiography (CTA) (Figure 2). 3. Patients met the Castor stent graft indications: presence of aortic arch disease with proximal lesions situated 15 mm distally to the left common carotid artery (LCCA) and 20 mm distally to the LSA, with extension into the LSA and a proximal landing zone of at least 15 mm.
Exclusion criteria: 1) patients with severe comorbidities that posed significant surgical risks, including advanced heart failure, significant renal insufficiency or uncontrolled coagulopathies; 2) patients with a life expectancy of less than 6 months due to other critical illnesses; 3) patients with anatomical conditions incompatible with the Castor stent graft, such as extremely large or small vessel diameters that could not accommodate the available stent sizes; 4) patients with a history of previous aortic arch surgeries that could complicate the placement and anchoring of the stent.
Although patients with different types of aortic arch diseases were included, strict inclusion and exclusion criteria ensured a relatively uniform cohort suitable for the Castor stent graft procedure. Consequently, the surgical technique was consistent across cases, with minor adjustments made only for specific anatomical complexities to optimize outcomes.
Surgical methods
Preoperative preparation and anesthesia: After induction of anesthesia using a combination of intravenous and inhalation agent, patients were placed in the supine position, disinfected and administered heparin at a dose of 1.0 mg/kg.
Catheter insertion and access: A 7F sheath was inserted through the left brachial artery, and a 5F sheath was inserted via the right brachial artery. An angiography catheter was then introduced through the right brachial artery into the ascending aorta to perform aortography and confirm the precise location of the lesions.
Stent selection criteria: Stent selection was based on preoperative CTA measurements, considering anatomical characteristics such as the proximal and distal landing zones and the orientation of the LSA. The Castor stent model was selected based on the diameter and length required to cover the lesion while ensuring secure anchoring in the landing zones. Measurements were also confirmed intraoperatively using angiography to ensure accurate stent sizing.
Guidewire and stent placement: After establishing vascular access from the left brachial artery to the right femoral artery, a transverse incision was made in the right inguinal region, and the femoral artery was dissected. The selected Castor stent graft was then inserted through the right femoral artery, with placement guided by real-time imaging. The direction-turnover technique was utilized to ensure that the stent fenestration aligned precisely with the aortic arch branches, with the stent automatically flipping to the correct position upon advancement. Re-angiography confirmed the positioning of the stent, showing unobstructed branch arteries and complete lesion coverage (Figure 3).
Unwrapping technique for guidewire management: To avoid guidewire entanglement, the unwrapping technique was applied when necessary. This involved retracting the stiff guidewire into the stent sheath to reduce tension and then gently guiding the branch wire to the LSA to maintain optimal placement. This step was crucial to ensure proper orientation and secure stent deployment.
Postoperative procedure: After confirming the stent position, all guidewires and catheters were removed, and the right inguinal incision was sutured layer by layer. Postoperatively, aspirin (100 mg) was administered to each patient to reduce the risk of thrombosis.
Equipment and consumables
The procedures used a 7F catheter for brachial artery access, 5F sheaths, and specialized angiography catheters. The Castor stent models were chosen based on individual patient anatomy. Additionally, contrast agents were employed during angiography to facilitate lesion visualization and stent placement.
Variables
The primary outcomes measured included: Operation time: Defined as the time from brachial artery puncture to the removal of all guidewires and catheters. Blood loss: Amount of blood lost during surgery. Complications: Including residual shunt, arrhythmia, hemolysis, embolism in the aortic arch, stent migration or detachment, and pericardial effusion. Postoperative CTA evaluation: Postoperative CTA was used to assess the morphology and stability of the stent and confirm the absence of endoleaks, displacement or other complications (Figure 4).
Statistical analyses
Data were collected from surgical records, patient medical records and imaging studies (CTA), with standardized measurement methods applied to ensure accuracy and comparability across all recorded outcomes. Additionally, descriptive statistics were used to summarize patient characteristics and procedural outcomes. Continuous variables were presented as mean ± standard deviation (SD) if normally distributed, or as median with 1st and 3rd quartiles (Q1–Q3) if non-normally distributed. Categorical variables were presented as counts and percentages. No inferential statistical tests were conducted, given the study’s preliminary nature and single-arm design.
Results
To evaluate the success of the Castor stent graft placement, we assessed intraoperative and postoperative outcomes related to stent positioning, hemodynamic stability and complication rates.
Intraoperative outcomes
Computer blood tube imaging confirmed that all stents were accurately positioned and completely covered the targeted lesions, with no significant deviation or endoleak observed. Additionally, all 3 branches of the aortic arch remained patent, and no cases required conversion to open thoracotomy. The average duration of surgery was 133.06 ±20.52 min. Intraoperative blood loss had a median of 50.0 mL (Q1–Q3: 20.0–50.0 mL), and no blood transfusions were required. Oxygen saturation remained stable between 95% and 100%, with controlled blood pressure showing no significant fluctuations. Various delivery sheath diameters, ranging from 6F to 10F, were utilized based on the anatomical requirements. Table 2 details the specific Castor stent models used. These findings indicated that the procedure was performed with minimal blood loss and stable patient vital signs, supporting the safety and effectiveness of the surgical approach.
Patient characteristics and hospital stay
The cohort consisted of 18 patients with diverse aortic arch pathologies: 11 patients (61.1%) were diagnosed with Stanford type B dissection, 3 (16.7%) with intramural hematoma, 2 (11.1%) with penetrating ulcers, 1 (5.6%) with a combination of penetrating ulcers and intramural hematoma, and 1 (5.6%) with an aortic arch aneurysm. The mean total hospital stay was 10.83 ±2.18 days, and the time in hospital post-surgery was 6.0 days (Q1–Q3: 5.0–7.0). These results demonstrated a manageable hospital recovery time, indicating that patients tolerated the procedure well and were able to be discharged in a reasonable timeframe.
Follow-up outcomes
At an average follow-up of 7.78 ±5.53 months, CTA reexaminations demonstrated that all Castor stent grafts remained securely positioned, with no evidence of displacement, detachment or occlusion. The lesions continued to be adequately covered, and there was no development of new lesions, endoleaks, or postoperative complications such as infective endocarditis. Notably, all patients reported that chest pain and tightness had either resolved or improved significantly, highlighting the procedure’s effectiveness in symptom relief and lesion management.
In summary, the intraoperative and follow-up results underscore the precision and stability of the Castor stent placement, with minimal complications, effective lesion coverage, and promising short-term outcomes for symptom relief and patient recovery.
Discussion
Advantages of Castor single-branch bracket
The Castor single-branch stent was specifically designed to maintain LSA blood flow during endovascular repair of aortic arch diseases, such as type B dissection. Preservation of LSA flow is critical as it reduces the risk of perioperative complications, including cerebral infarction and spinal cord ischemic paraplegia.17
The Castor stent offers unique structural benefits compared to traditional straight stents. Its single-branch design, anchored by radial support, provides stability almost perpendicular to aortic blood flow, while simultaneously benefiting from the anchoring force generated by blood flow and blood pressure in the LSA branch. This dual anchoring mechanism enhances stent stability and minimizes migration risks.18 Moreover, the size and positioning of the Castor stent are customized based on preoperative CTA and intraoperative angiographic measurements.14 This approach enables precise deployment, making the Castor stent an ideal solution for patients with complex aortic arch lesions who are unsuitable for open surgery.
Application and impact of innovative technologies
To optimize the placement of the Castor stent, we employed 2 innovative techniques: the direction-turnover technique and the unwrapping technique. The direction-turnover technique, proposed by Professor Qingsheng Lu from Changhai Hospital, leverages spatial inversion to control the stent’s fenestration orientation during deployment.19 As depicted in Figure 5, the surgeon holds the anterior grip at the 6 o’clock position without rotation, ensuring that the white marker aligns perpendicularly to the ground (Figure 5A). This alignment ensures that the fenestration remains correctly positioned as the stent advances through the aortic arch (Figure 5B). Upon reaching the ascending aorta, the fenestration automatically flips to the 12 o’clock position, aligning with the branches of the aortic arch (Figure 5C). This transformation simplifies the complex 3-dimensional alignment challenge, enabling a more intuitive and accurate stent placement.
The unwrapping technique, used to address guidewire entanglement, involves retracting the stiff guidewire into the stent sheath while maintaining gentle tension on the branch guidewire (Figure 6). This method allows the branch stent to enter the LSA unobstructed, thus preventing potential cerebral ischemia and reducing the risk of deployment issues. These complementary techniques reduce procedural complexity, improve safety and enhance the reliability of Castor stent implantation, thereby making the procedure more accessible to surgeons across a range of experience levels.
Postoperative outcomes and complications
The short-term outcomes observed in this study demonstrate the effectiveness and safety of the combined approach. All 18 patients successfully underwent Castor stent implantation without the need for conversion to open surgery. Over a follow-up period of 7.78 ±5.53 months, CTA imaging confirmed stable stent positioning with no migration, endoleaks or significant complications. Patients also reported relief from chest pain and tightness, with a mean hospital stay of 10.83 ±2.18 days and a discharge period averaging 6.28 ±1.36 days, suggesting a favorable recovery profile.
Compared to recent studies, the Castor stent approach demonstrates potential advantages. For instance, a study by Shu et al.20 reported an 11% incidence of type I endoleaks using the chimney technique, whereas no endoleaks were observed in our study. These findings suggest that the Castor stent approach may provide a safer and more efficient alternative for complex aortic arch repairs; however, larger, long-term studies are needed to validate these results.
Noteworthy, factors such as patient age, disease severity and anatomical complexity may influence surgical outcomes, with older or high-risk patients potentially facing different recovery trajectories and higher risks of complications, such as postoperative cerebral infarction or spinal cord ischemia. Future studies should further investigate these variables to refine patient selection and develop effective prevention strategies for such complications. Moreover, as this technique becomes more widely adopted, challenges related to procedural complexity and operator training will need to be carefully addressed. Successful implementation requires expertise in spatial orientation and guidewire manipulation, underscoring the need for comprehensive training and advanced imaging. Addressing these factors will support broader clinical application, especially in high-risk cases.
Limitation of the study and future research directions
While this study provides promising preliminary data, it has several limitations. First, as a single-arm study without a control group, we were unable to perform comparative analyses or assess the relative efficacy of the direction-turnover and unwrapping techniques against alternative methods like the chimney or fenestration techniques. Future studies with a comparative or controlled design would provide stronger evidence for the efficacy of these techniques.
Second, the small sample size (18 patients) limits the generalizability of our findings. Although no major adverse events or failure cases were observed in this cohort, the small sample may not capture the full spectrum of potential complications, especially in more diverse patient populations. Expanding the sample size in future studies would enhance the external validity and reliability of the results and allow for a more comprehensive assessment of safety.
Additionally, there was a notable sex imbalance in our sample (17 men and 1 woman). This disproportion reflects the higher prevalence of aortic arch disease among men, as reported in previous studies.21 However, it may limit the applicability of our findings to female patients, who may have different outcomes or complication rates. Future research should aim for a more balanced sample to improve the generalizability of the results across both sexes.
Lastly, the follow-up period was relatively short, averaging 7.78 months, which limits our ability to assess the long-term safety and durability of the Castor stent. Future studies should incorporate a follow-up period of at least 2 years to evaluate the long-term efficacy and potential late complications, including stent displacement, restenosis and other potential adverse events.
By addressing these limitations in future research, we can establish a stronger foundation for the clinical application of the Castor stent with direction-turnover and unwrapping techniques, particularly for high-risk patients who are unsuitable for open surgery.
Conclusions
The Castor single-branch stent represents an effective treatment option for patients with aortic arch disease who are unsuitable for thoracotomy and meet the specific criteria for endovascular repair. The application of the direction-turnover and the unwrapping techniques during stent placement demonstrated the ability to enhance surgical precision, improve the success rate and minimize guidewire entanglement. Short-term outcomes demonstrate safe and reliability, with promising potential for application. Further studies with larger sample sizes and extended follow-up are warranted to confirm these findings and evaluate long-term efficacy.
Supplementary data
The supplementary materials are available at https://doi.org/10.5281/zenodo.15208395. The package includes the following files:
Supplementary Table 1 Analysis of normal distribution for continuous variables.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.

















.png)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)