Abstract
Background. The potential role of interleukin-6 (IL-6) in coronavirus disease 2019 (COVID-19) pneumonia provides the rationale for investigating IL-6 signaling inhibitors.
Objectives. To evaluate and report treatment responses to tocilizumab (TCZ) in COVID-19 patients and compare mortality outcomes with those of standard care.
Materials and methods. Patients hospitalized with a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, diagnosed with reverse transcription polymerase chain reaction (RT-PCR) between March 2020 and April 2021, were enrolled in this single-center retrospective cohort study. Propensity score matching was performed in order to reduce confounding effects secondary to imbalances in receiving TCZ treatment.
Results. A total of 364 patients were included in this study. Two hundred thirty-six patients received standard care, while 128 patients were treated with TCZ in addition to standard care (26 (20.3%) patients received a dose of 400 mg intravenously once, while 102 (79.7%) patients received a total dose of 800 mg intravenously). In the propensity score-matched population, less noninvasive mechanical ventilation (p = 0.041) and mechanical ventilation support (p = 0.015), and fewer deaths (p = 0.008) were observed among the TCZ-treated patients. The multivariate adjusted Cox regression model showed a significantly higher survival rate among TCZ patients compared to controls (hazard ratio (HR): 0.157, 95% confidence interval (95% CI): 0.026–0.951; p = 0.044). The hazard ratio for mortality in the TCZ group was 0.098 (95% CI: 0.030–0.318; p = 0.0001 using log-rank test).
Conclusions. This study determined that TCZ treatment in COVID-19 patients was associated with better survival, reduced need for mechanical ventilation and reduced hospital-associated mortality.
Key words: pneumonia, tocilizumab, COVID-19, cytokine storm, mortality
Background
In December 2019, a novel coronavirus was identified in Wuhan, China. It had clinical characteristics comparable to those of severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) and Middle East respiratory syndrome coronavirus (MERS-CoV).1 This new coronavirus form, known as SARS-CoV-2, quickly spread around the globe, with the first case discovered in Turkey on March 11, 2020. As of September 12, 2021, there were 6,039,857 confirmed coronavirus disease 2019 (COVID-19) cases and 52,860 COVID-19-related deaths.2
Coronavirus disease 2019 begins with a period of rapid viral replication, followed by a 2nd phase controlled by the host immunological response.1 Cytokine storms mediated by proinflammatory cytokine overproduction have been recognized in the vast majority of critically ill COVID-19 patients.3 Cytokine storms cause cardiovascular collapse, multiple organ dysfunction and death. Patients at this stage have abnormal inflammatory markers, such as increased levels of serum ferritin, interleukin-6 (IL-6), and C-reactive protein (CRP).4 Higher levels of serum IL-6 have been linked to increased SARS-CoV-2 viremia, extended viral RNA shedding, progression to mechanical ventilation, and death.5, 6 These findings led us to hypothesize that blocking the IL-6 receptor could terminate the inflammatory process at a critical point. As a result, early detection, treatment and prevention of cytokine storms may be vital for patients.
The significant role of IL-6 in COVID-19 pneumonia justifies further research into IL-6 signaling inhibitors.7, 8 Tocilizumab (TCZ) is a monoclonal antibody that targets the IL-6 receptor alpha and is used to treat inflamatory diseases such as rheumatoid arthritis, giant cell arteritis, and systemic sclerosis-associated interstitial lung disease.9 In cases of severe COVID-19 pneumonia, patients who received TCZ were shown to have better outcomes, and retrospective observational cohort studies revealed an immediate decrease in fever, decreased need for oxygen therapy and mechanical ventilation, as well as an improvement in lung symptoms.10, 11, 12, 13, 14
Objectives
The goal of this retrospective cohort study was to describe the therapeutic response to TCZ in COVID-19 patients and compare mortality outcomes to those associated with standard therapy.
Materials and methods
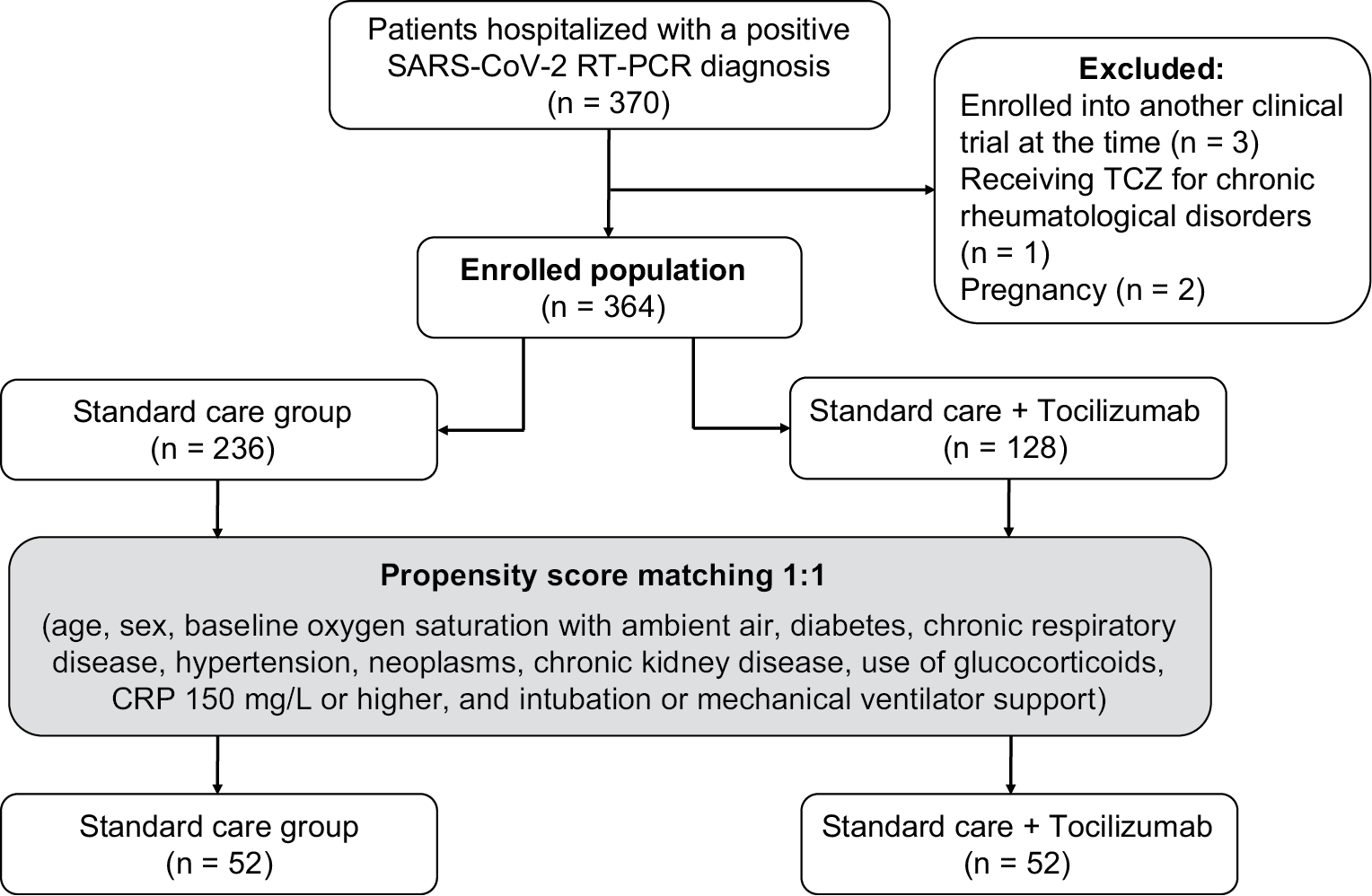
Between March 2020 and April 2021, adult patients (18 years and older) hospitalized with a positive SARS-CoV-2 reverse transcription polymerase chain reaction (RT-PCR) diagnosis at the Uludağ University Faculty of Medicine in Bursa, Turkey, were enrolled in this single-center retrospective cohort study. Pregnant women, patients enrolled in other clinical trials and patients receiving TCZ for chronic rheumatic disorders were excluded. The study protocol is summarized in Figure 1.
Each patient provided written informed consent prior to the inclusion in the study. The study followed the principles of the Declaration of Helsinki and was approved by the Uludağ University Faculty of Medicine Clinical Research Ethics Committee (approval No. 2020-23/11), as well as the Ministry of Health’s of the Republic of Turkey Ethical Committee.
Data collection
The electronic health records database at the hospital included sociodemographic information, clinical presentation, comorbid conditions, chest computed tomography (CT) findings, laboratory results, therapies, and their variables. Comorbidities were defined as those diagnosed prior to COVID-19 hospitalization.
Lymphocyte, eosinophil, ferritin, D-dimer, CRP, and procalcitonin parameters were recorded at baseline, before the TCZ treatment, and on the 1st, 3rd, 5th, 7th, and 14th day of treatment. The duration of hospitalization, number of days from hospitalization to death and secondary infection rates were recorded. The main endpoint was intubation or in-hospital mortality.
Definitions
Possible COVID-19 instances were diagnosed according to the national guidelines of Turkish Ministry of Health.2, 15 Nasopharyngeal swabs were taken for real-time RT-PCR when patients were admitted. Chest X-rays taken at admission were reviewed, and chest CT patterns and distributions characteristic of COVID-19 infection were carefully defined in accordance with the Radiological Society of North America’s expert consensus statement, which proposes 4 categories for standardized COVID-19 reporting (“typical appearance,” “indeterminate appearance,” “atypical appearance,” and “negative for pneumonia”).16 A chest radiologist and an experienced pulmonologist reviewed each probable COVID-19 patient’s chest CT.
Hospital care and treatment of patients
From hospital admissions to treatment protocols, all clinical decisions adhered to the national guidelines published by the Turkish Ministry of Health.2 Patients were observed until the completion of the clinical monitoring period, which was described as complete recovery, discharge from hospital with SpO2 greater than 94% on room air, or death.
In the standard care group, the patients received favipiravir (1600 mg twice daily as a loading dose, followed by 600 mg twice daily as a maintenance dose); antibiotics were also administered as an initial treatment to account for the possibility of a bacterial etiology. Convalescent plasma was administered within 7 days of symptom onset in selected patients. Severely ill COVID-19 patients who required supplemental oxygen or ventilator support were administered 6 mg of dexamethasone daily for 10 days or until discharge.
Tocilizumab was added to standard therapy in patients who had clinical and laboratory findings such as persistent fever despite treatment, continuing to increase or constantly high proinflammatory cytokines and inflammatory markers, elevated ferritin, lymphopenia and thrombocytopenia, or elevated D-dimer.
Statistical analyses
The IBM SPSS Statistics for Windows, v. 23.0 software (IBM Corp., Armonk, USA) was used to conduct the statistical analyses. The Shapiro–Wilk test was used to ascertain the distribution of the variables. When the data were normally distributed, they were shown as mean and standard deviation (SD). When the data were not normally distributed, they were presented as median (interquartile range (IQR)). The categorical characteristics were given as numbers (%). To compare continuous outcome variables between the groups, we used the independent samples t-test for normally distributed data and the Mann–Whitney U test for non-normally distributed data. The Pearson’s χ2 test was used to compare categorical variables. The Friedman tests were employed to identify if significant changes in the lymphocyte, eosinophil, ferritin, D-dimer, CRP, and procalcitonin variables were observed due to incorrect parametric test assumptions (non-normal distribution).
We used propensity score matching to eliminate confounding effects caused by imbalances in TCZ treatment approval, inherent in a retrospective cohort analysis. To begin with, we calculated a propensity score for each patient in order to receive TCZ treatment using multivariable logistic regression with the confounding variables (age, sex, baseline oxygen saturation with ambient air, diabetes, chronic respiratory disease, hypertension, malignancy, chronic kidney disease, use of glucocorticoids, CRP 150 mg/L or higher, and intubation or mechanical ventilator support). The Hosmer–Lemeshow test was used to determine the multivariable logistic regression model’s fit. Then, using NCSS 2019 statistical software (NCSS, Kaysville, USA), we employed nonparametric nearest neighbor matching of propensity scores to establish a matched cohort in a 1:1 ratio, pairing patients treated with TCZ with those who were not. To identify risk factors that are thought to be important in predicting mortality, the variables reported in the univariate studies were first investigated using univariate Cox regression. Then, the variables meeting the p < 0.25 threshold were included in the multivariate Cox regression model. When the relevant variables were analyzed using Cox regression, it was determined that age, hypertension, baseline SpO2 in ambient air, need for intubation, and receiving TCZ met the p < 0.25 criterion.17 The enter selection method was used to choose variables, and the results of the analysis were shown. The hazard ratios (HRs) and 95% confidence intervals (95% CIs) were summarized. The proportional hazard assumption was checked by producing a time variable (T-COV).
The survival rates of patients treated with TCZ in addition to standard therapy (TCZ group) and patients treated with standard therapy alone (standard treatment group) were determined using a Kaplan–Meier plot, with group (TCZ compared to standard treatment) as the between factor, death as the event, and time to death or discharge as the time variable. To determine statistical significance, an overall 5% type I error threshold was applied.
Results
A total of 364 patients were included in this study. Two hundred thirty-six patients received standard care, while 128 patients were treated with TCZ in addition to standard care (26 (20.3%) patients received a dose of 400 mg intravenously once, while 102 (79.7%) patients received a total dose of 800 mg intravenously). Baseline demographic details, clinical characteristics, and laboratory and radiology findings are reported in Table 1 and Table 2, as unmatched and propensity score-matched.
Tocilizumab was used more frequently in male patients (93 (72.7%) compared to 124 (52.5%), p < 0.001). It was administered for a median of 12 (5–36) days after the start of patient-reported symptoms, a median of 6 days (1–23) from the date of hospitalization, and a median of 1 day (0–15) from the date of intensive care unit (ICU) support. Of the 364 patients, 78 (21.4%) died, including 52 (40.6%) of the 128 that received TCZ and 26 (11.0%) of the 236 that did not receive TCZ. Fifty-three (41.4%) of the 128 patients who received TCZ were started on it after intubation. Of these, 52 (98.1%) died, while 1 (1.9%) required extracorporeal membrane oxygenation (ECMO) support and was extubated during the follow-up.
In the unmatched population, patients who received TCZ had significantly longer symptom duration, longer hospital stay, lower baseline oxygen saturation, and more dyspnea than patients who did not receive TCZ (median (IQR): 5 (4) days) compared to 3 (5), p < 0.001; 16 11) compared to 7 (6), p < 0.001; 92 (7) compared to 96 (6), p < 0.001; 72 (56.3%) compared to 89 (36.9%), p < 0.001, respectively). In the propensity score-matched population, patients who received TCZ had significantly longer symptom duration and longer hospital stay than patients who did not (6 (3) compared to 3 (5), p = 0.002; 14 (9) compared to 8 (5), p < 0.001, respectively).
Among both the unmatched and propensity score-matched patients, there were significant differences between groups that did and did not receive TCZ in terms of typical chest CT images (p = 0.008 and p = 0.033, respectively). In addition, TCZ-treated patients had significantly lower lymphocyte, eosinophil and platelet levels than patients who were not treated with TCZ (Table 2).
In the unmatched population, patients who received TCZ had more noninvasive mechanical ventilation (NIMV), high-flow nasal oxygen (HFNO) and mechanical ventilation requirements, as well as more deaths than patients who did not recieve TCZ (p < 0.001 for each). In the propensity score-matched population, conversely, less NIMV (p = 0.041) and mechanical ventilation support (p = 0.015) and fewer deaths (p = 0.008) were observed among the TCZ-treated patients. Additionally, in the propensity score-matched population, more TCZ-treated patients required HFNO than non-TCZ-treated patients (17 (32.7%) compared to 5 (9.6%), p = 0.004).
The multivariate adjusted Cox regression model (adjusted for age, hypertension, baseline oxygen saturation with room air, and intubation) revealed that TCZ patients had a significantly higher survival rate than patients who did not receive TCZ (HR: 0.157, 95% CI: 0.026–0.951; p = 0.044; Table 3). Meanwhile, the risk of death was 5.3 times higher (p = 0.017) due to hypertension and 18.5 times higher (p < 0.001) when intubation was required.
The Kaplan–Meier curves for time to death are shown in Figure 2. The hazard ratio for mortality in the TCZ group was 0.098 (95% CI: 0.030–0.318; p = 0.0001 using log-rank test).
Considering the pharmacodynamics of TCZ, an immediate effect on inflammatory indices is expected. Patients in the TCZ group were monitored for 14 days after the beginning of therapeutic interventions. Distributions of lymphocyte, eosinophil, ferritin, D-dimer, CRP, and procalcitonin parameters at baseline, before TCZ treatment, and on the 1st, 3rd, 5th, 7th, and 14th day of treatment are shown in Table 4.
Of the 128 patients who received TCZ, 35 (27.3%) developed a bacterial infection, 4 (3.1%) a fungal infection and 2 (1.6%) a viral infection (cytomegalovirus viremia) during hospitalization. Positive sputum cultures were identified in 25 (19.5%) patients.
Discussion
This single-center retrospective cohort study aimed to evaluate therapeutic responses to TCZ in COVID-19 patients and compare mortality outcomes to those associated with standard therapy. Receiving TCZ was associated with a decrease in hospital-related mortality in patients hospitalized with COVID-19. However, of the 53 patients who received TCZ after intubation, 52 died. Among the general population of the study, TCZ was only administered to clinically severe cases. Therefore, in unmatched analyses, the need for respiratory support and mortality rates were found to be higher in TCZ-treated patients compared to those who received standard care without TCZ. The propensity score-matched model adjusted for the factors such as age, gender, basal oxygen saturation with room air, diabetes, chronic lung disease, hypertension, malignancy, kidney failure, steroid use, CRP of 150 mg/L or more, and intubation or mechanical ventilator support determined that patients who received TCZ required less mechanical ventilation support and had lower mortality rates.
Cytokine storm is a term that refers to an out-of-control inflammatory response and impaired immune system function induced by infection, certain drugs and other reasons such as malignant tumors or rheumatic diseases. Severe acute respiratory syndrome coronavirus 2 attaches to alveolar epithelial cells and subsequently activates both the innate and adaptive immune systems, resulting in the release of a variety of cytokines, including IL-6. Additionally, these proinflammatory substances enhance vascular permeability, resulting in a flood of fluid and blood cells into the alveoli, which can lead to shortness of breath and potentially, respiratory failure.18 Interleukin 6 is a critical component of the cytokine storm. It is typically reported in individuals with severe COVID-19 infection and found at significantly higher levels in these patients than in patients with less severe forms of the disease.18 In the propensity score-matched population, patients who received TCZ had significantly longer hospital stays than patients who did not receive it. Since TCZ is administered to clinically severe patients, longer durations of hospitalization in this patient population are expected.
In both the unmatched and propensity score-matched groups, patients who received TCZ had significantly lower lymphocyte, eosinophil and platelet levels than those who did not receive TCZ. The induction of cytokine storm by IL-6 results in a robust inflammatory response manifested by an increase in CRP and procalcitonin levels, a decrease in lymphocyte counts and stimulation of the coagulation pathway, as demonstrated by elevated D-dimer levels and hypoxia.19 It has been observed that eosinophils undergo considerable changes during the early stages of COVID-19 and are more sensitive to disease diagnosis than lymphocytes. Additionally, recovered patients experience a dynamic eosinophil recovery process, and peripheral blood eosinophils are significantly lower in deceased patients.20 Patients in the TCZ group were monitored for 14 days from the beginning of therapeutic interventions. Consistent with previous studies,21, 22 CRP, ferritin and D-dimer values decreased toward the normal range, while lymphocyte and eosinophil counts increased. In the groups of overall and discharged patients, a decrease was observed in procalcitonin levels at the follow-up after the TCZ treatment. Conversely, in the group of patients who died, there was an initial decrease followed by an increase in procalcitonin levels on the 14th day.
In a randomized clinical trial, TCZ administered with remdesivir did not shorten the time to hospital discharge in patients with severe COVID-19 pneumonia compared to placebo plus remdesivir group.23 It was reported that in subjects with severe COVID-19, the use of both TCZ and systemic corticosteroid therapy compared to no TCZ treatment reduced the risk of mortality.24 For severe COVID-19 patients, the addition of TCZ to the standard of care may reduce mortality and the need for mechanical ventilation.25 A meta-analysis that included 25 peer-reviewed publications determined that TCZ treatment is related to a decreased risk of mortality and the need for mechanical ventilation, as well as a better prognosis in COVID-19 patients, particularly those who are critically ill.26
In the unmatched population, patients who received TCZ had greater NIMV, HFNO, mechanical ventilation requirements, and mortality. On the contrary, in the propensity score-matched population, less NIMV and mechanical ventilation support were required, and there were fewer deaths in the TCZ-treated patients. In the propensity score-matched population, there was a greater need for HFNO in patients who received TCZ treatment. Stone et al. showed that TCZ was ineffective in preventing intubation or death in moderately ill COVID-19 patients.27 Another study indicated that treating individuals who have severe COVID-19 pneumonia with TCZ might reduce the risk of needing invasive mechanical ventilation and mortality.28
The multivariate adjusted Cox regression model showed that TCZ was associated with an 84% reduction in the risk of in-hospital death. However, the risk of death increased 5.3 times with hypertension and 18.5 times with intubation. The survival probability of TCZ-treated patients was significantly higher than that of untreated patients. In a meta-analysis, the administration of IL-6 antagonists was found to be associated with lower all-cause mortality 28 days after randomization.29 It has been reported that the relative risk of death is increased two-fold among patients with hypertension compared to patients without hypertension.30
Of the 128 TCZ-treated patients, 35 (27.3%) developed a bacterial infection, 4 (3.1%) a fungal infection and 2 (1.6%) a viral infection (cytomegalovirus viremia) while hospitalized. Positive sputum cultures were identified in 25 (19.5%) patients. Keske et al. detected secondary bacterial infections among 9 (41%) of the 22 patients who were admitted to the ICU and treated with TCZ.14 A meta-analysis of serious adverse events from 23 clinical trials concluded that the risk of secondary infection after 28 days was comparable between patients treated with IL-6 antagonists (750/3428; 21.9%) and those treated with standard care or placebo (330/1787; 17.6%).29 A single-center investigation found that patients treated with TCZ were more than twice as likely to develop a superinfection as untreated controls (54% compared to 26%), owing principally to a significant increase in ventilator-associated pneumonia (45% compared to 20%).31
Limitations
Although these data are retrospective and observational, we used propensity score matching to exclude confounding effects caused by imbalances in TCZ treatment. The limitations of this study include a lack of the evaluation of the secondary infection in patients who did not receive TCZ, and a lack of measurement of the IL-6 levels of the patients. In addition to the administration of TCZ according to the institutional guidelines, it was thought that there might be an indication bias, because the clinician plays an important role in the treatment decision.
Conclusions
This study concluded that TCZ treatment in patients with COVID-19 was associated with better survival, reduced need for mechanical ventilation and reduced hospital-associated mortality.